We have another great case in our Fellows’ Case Files coming today from UMass Chan. Listen in for a great discussion about a fascinating case with interesting physical exam and radiographic findings.
Meet Our Guests
Dr. Jen Kodela completed her residency training at UMass Memorial Medical Center and is currently a third year PCCM fellow at UMass Chan.
Dr. Ariel McKenna completed her residency training at Maine Medical Center and is also currently a third year PCCM fellow at UMass Chan.
Dr. Will Wong is an Assistant Professor of Medicine and is the Program Director of the PCCM fellowship at UMass Chan
Case Presentation
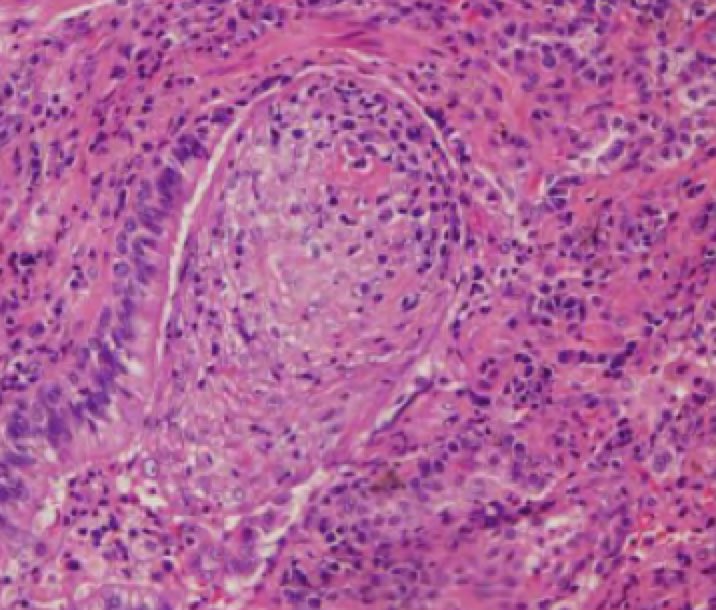
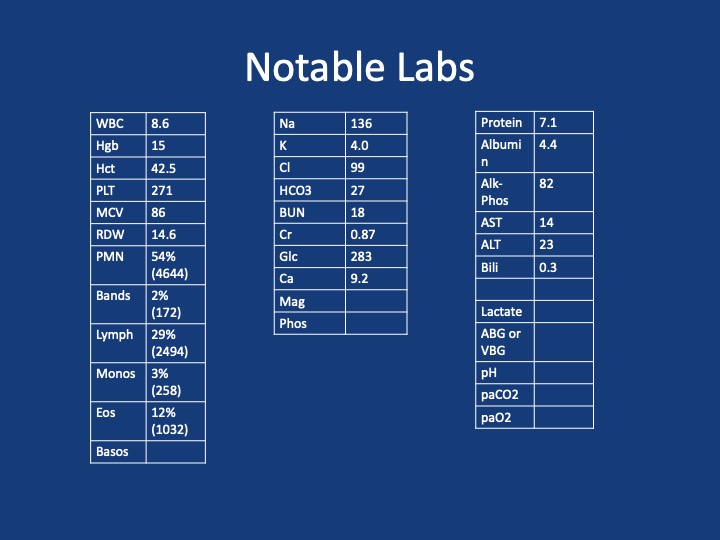
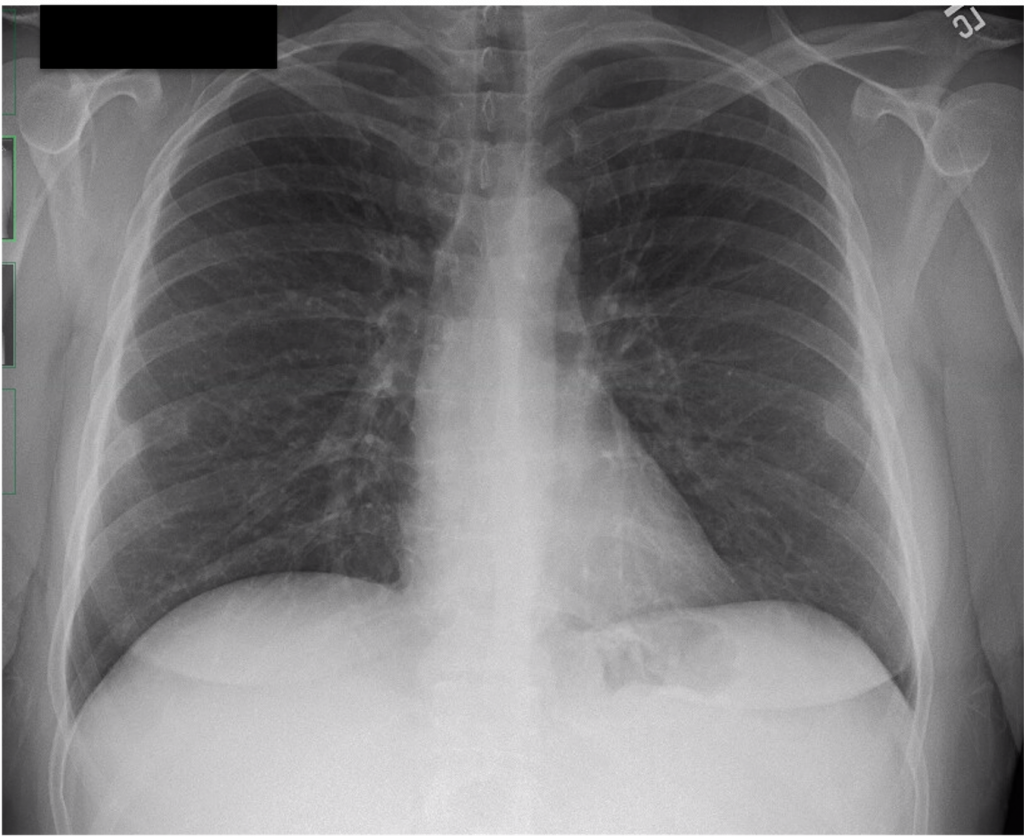
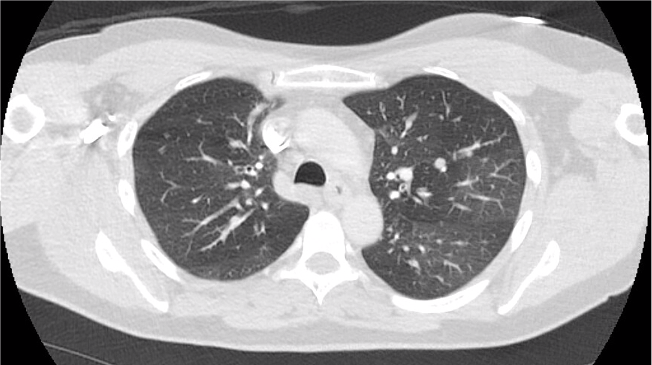
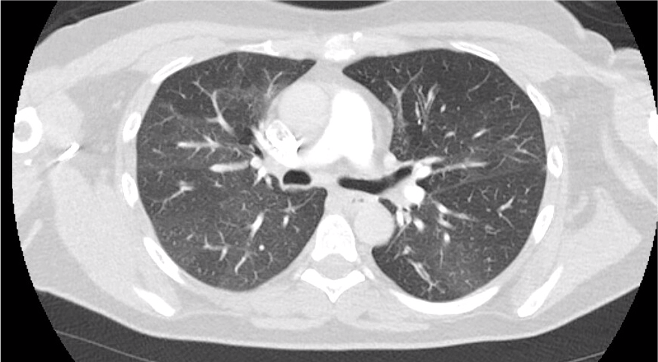
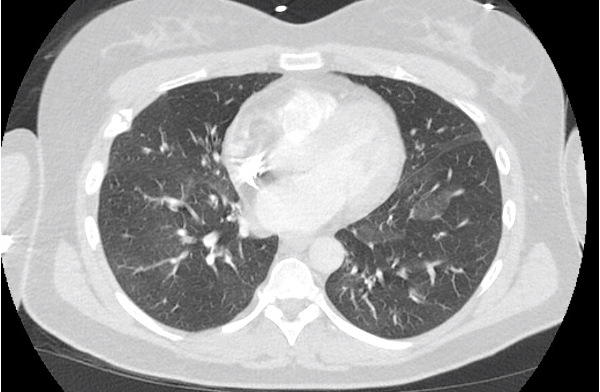
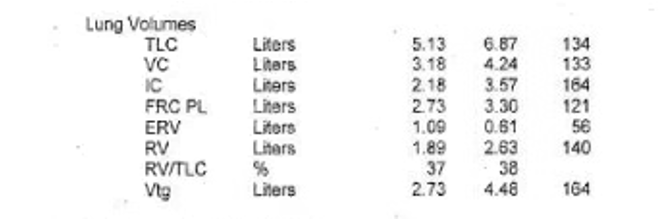
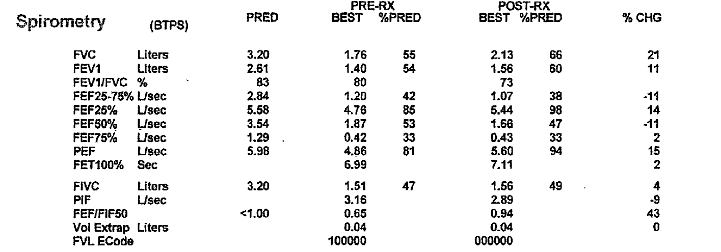
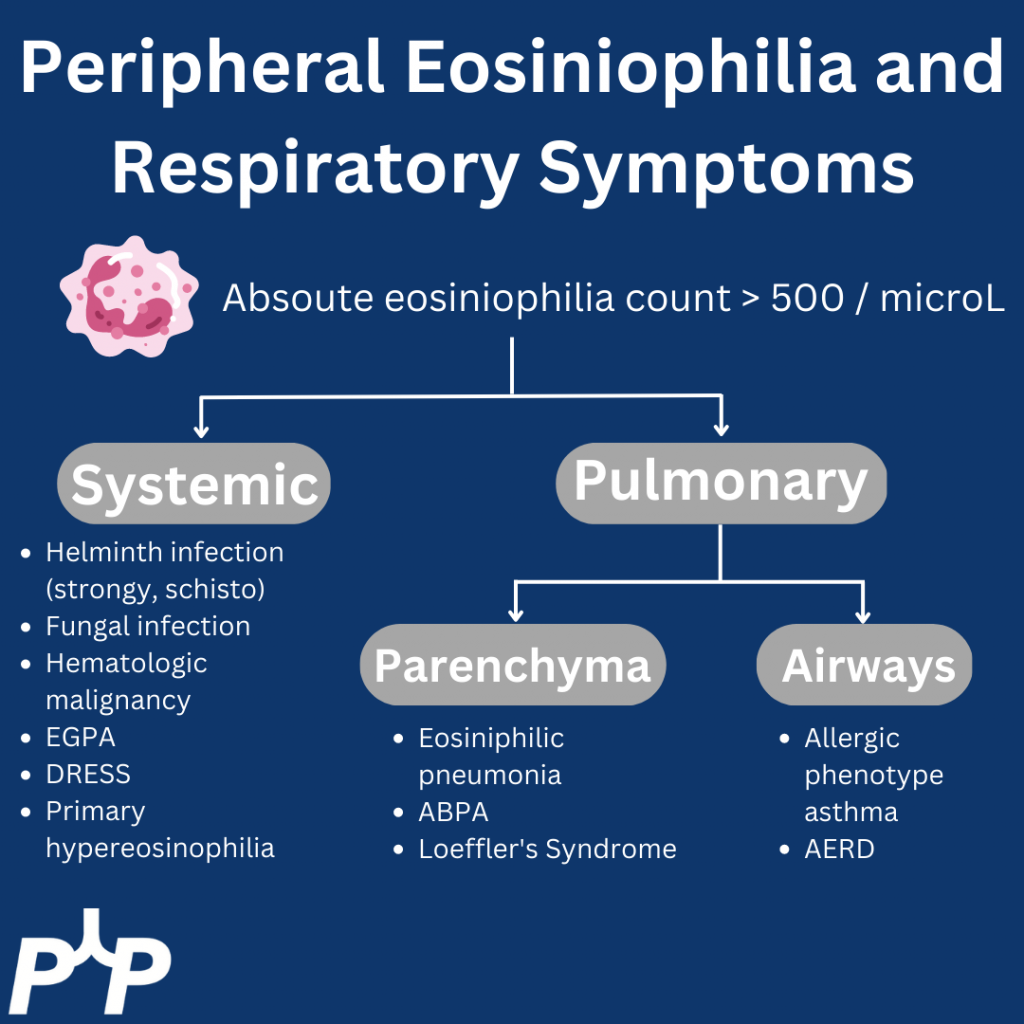
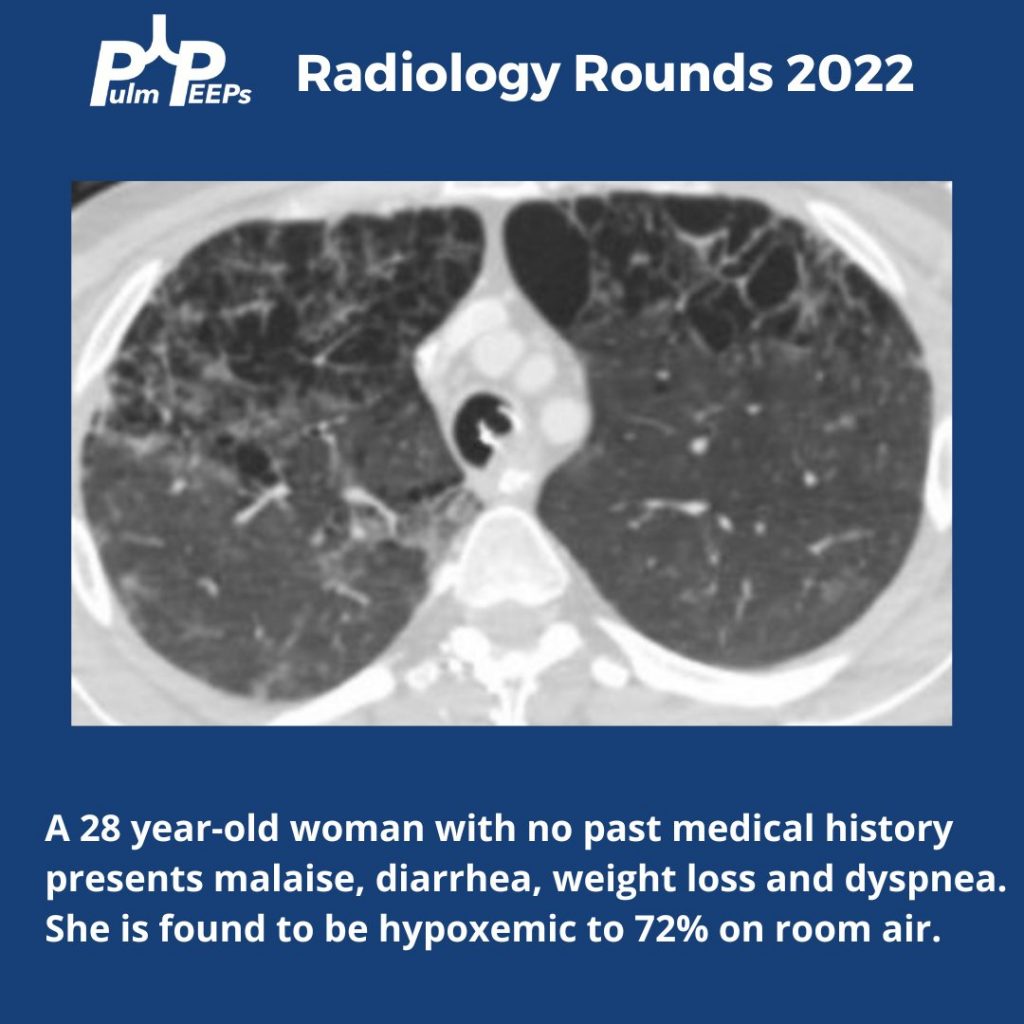
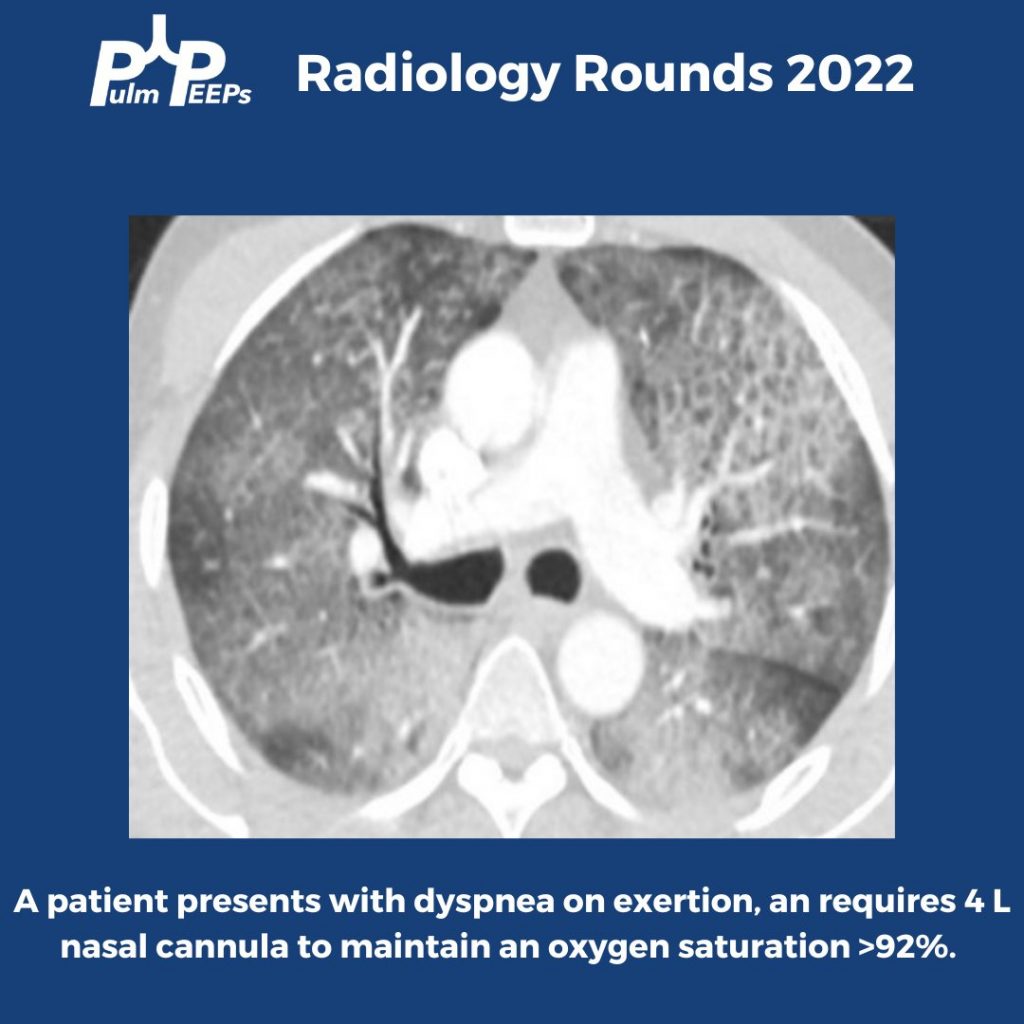
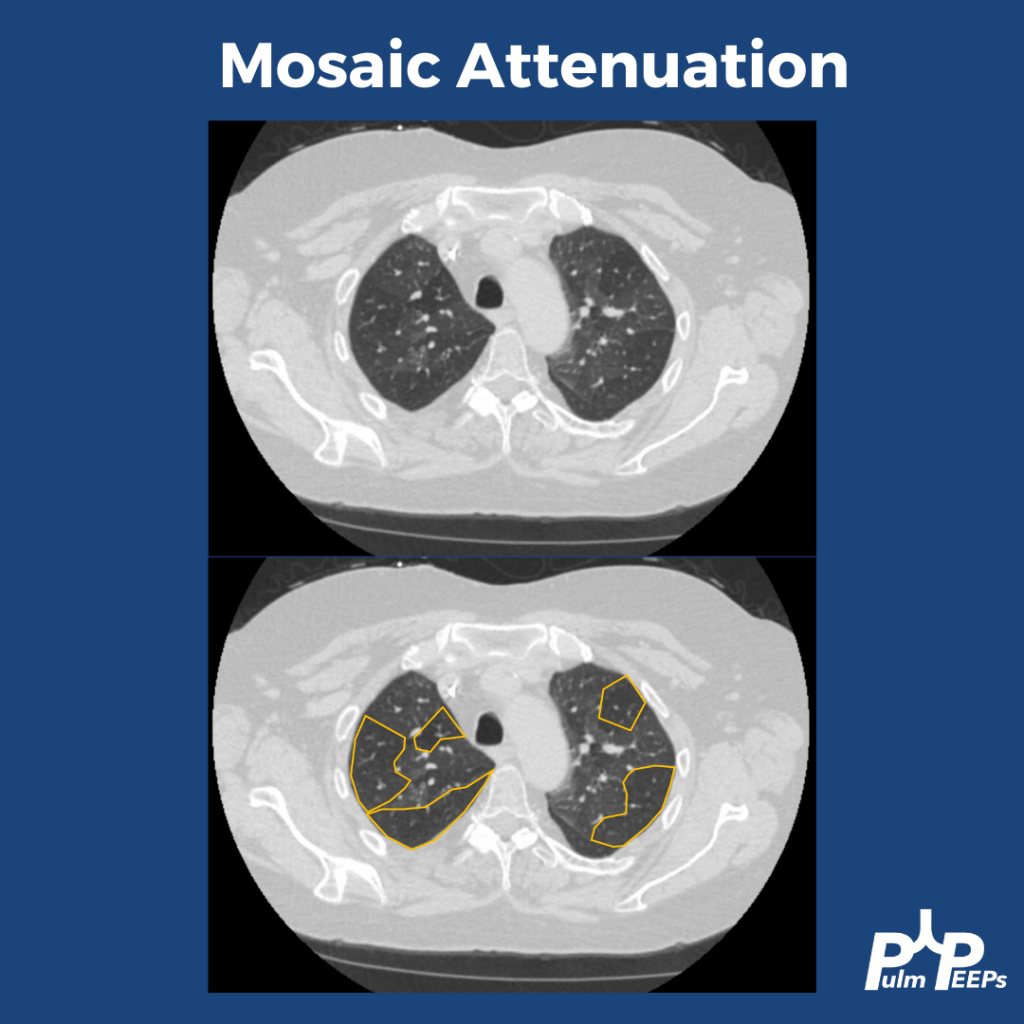
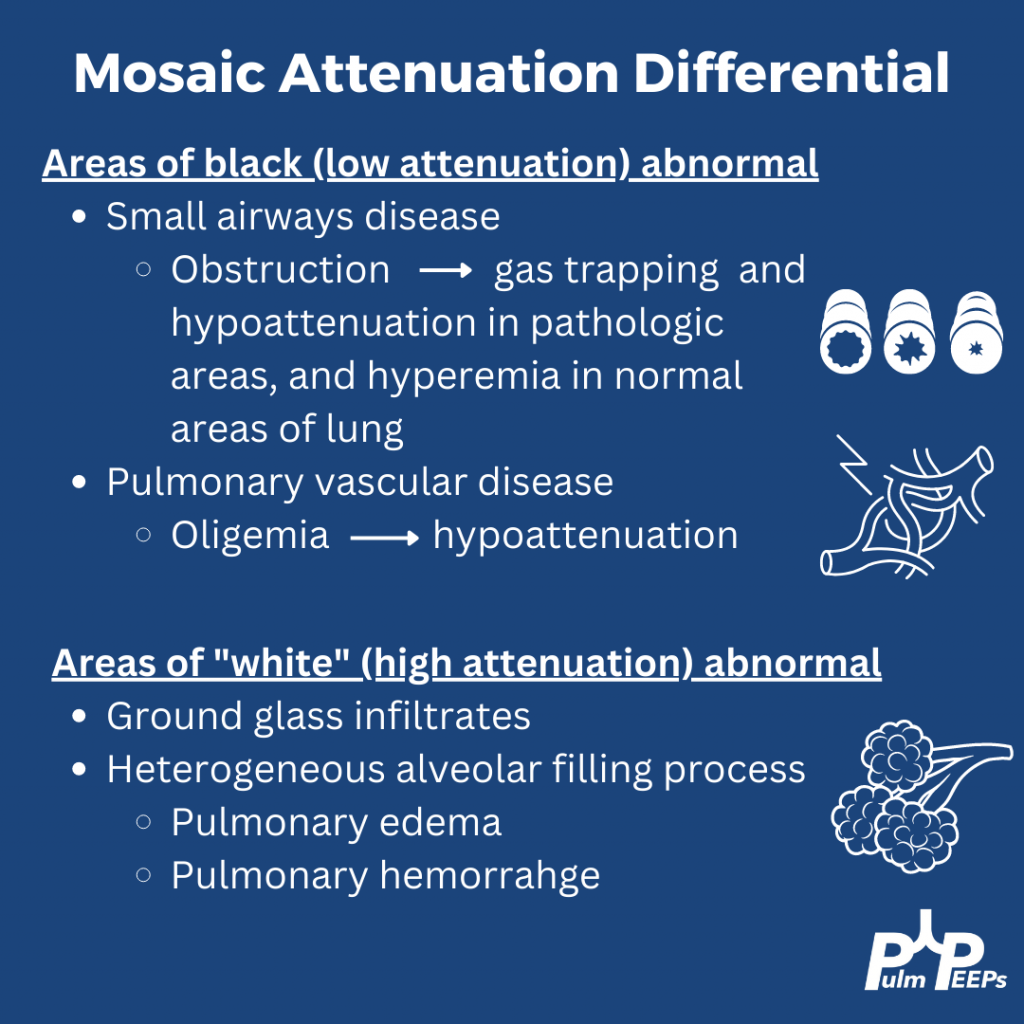
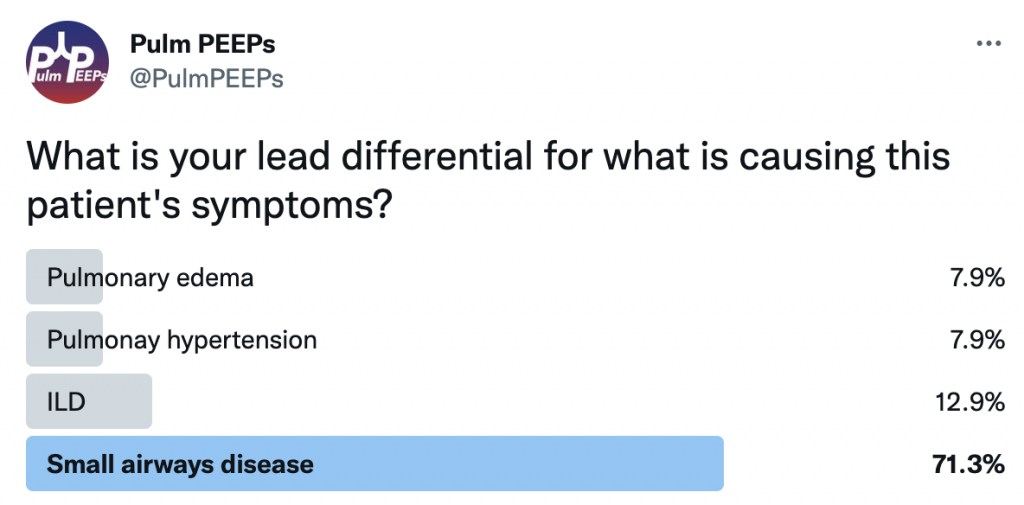
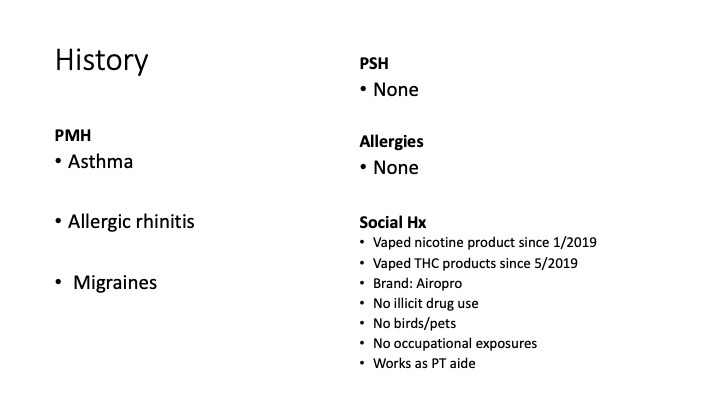
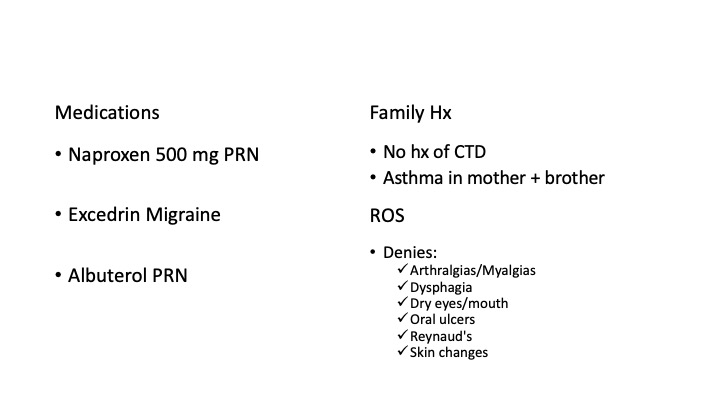
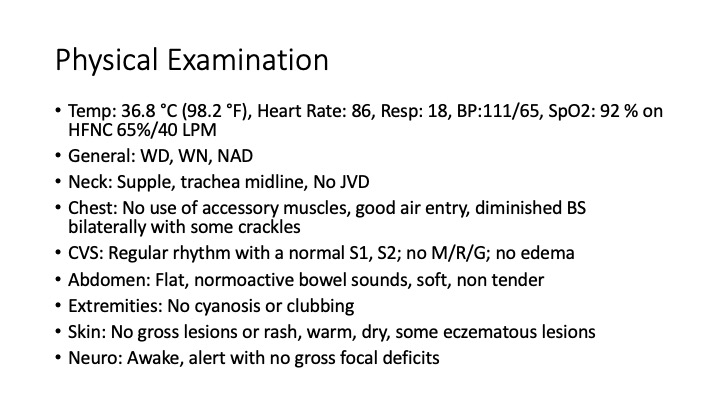
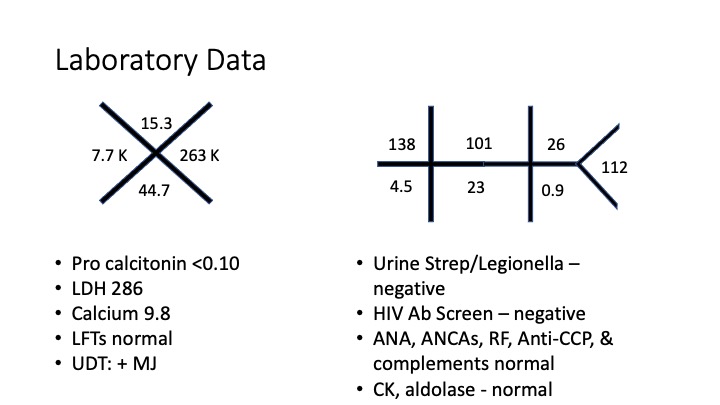
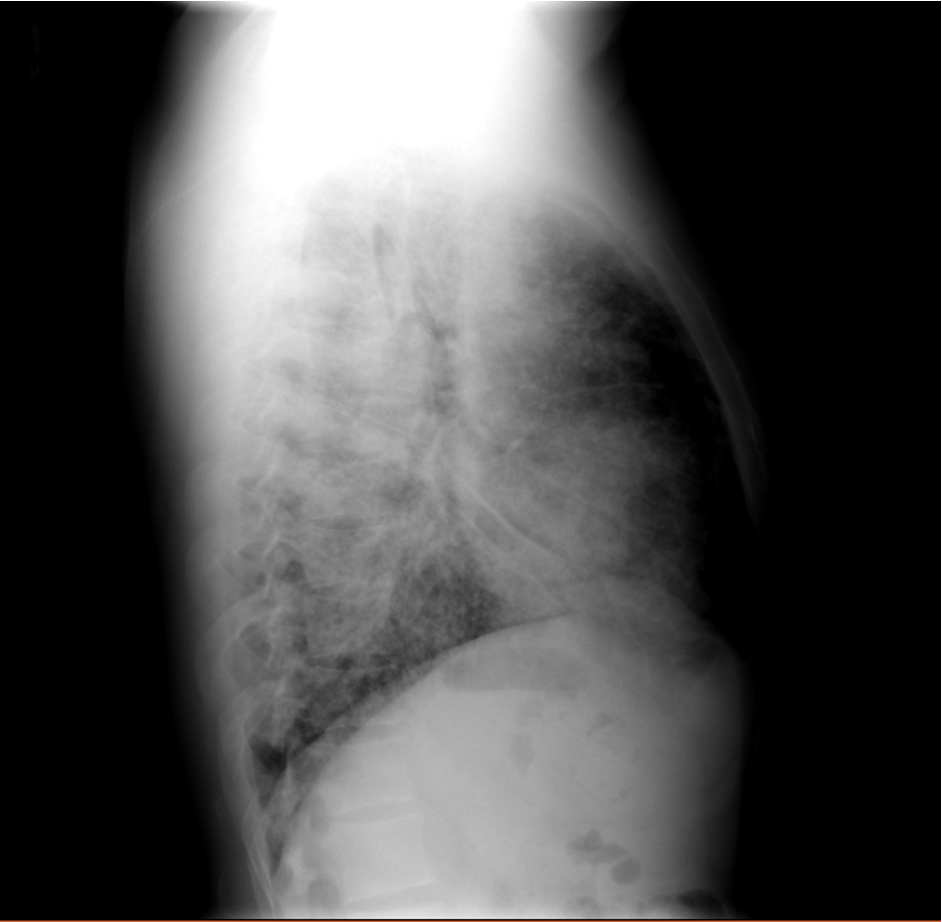
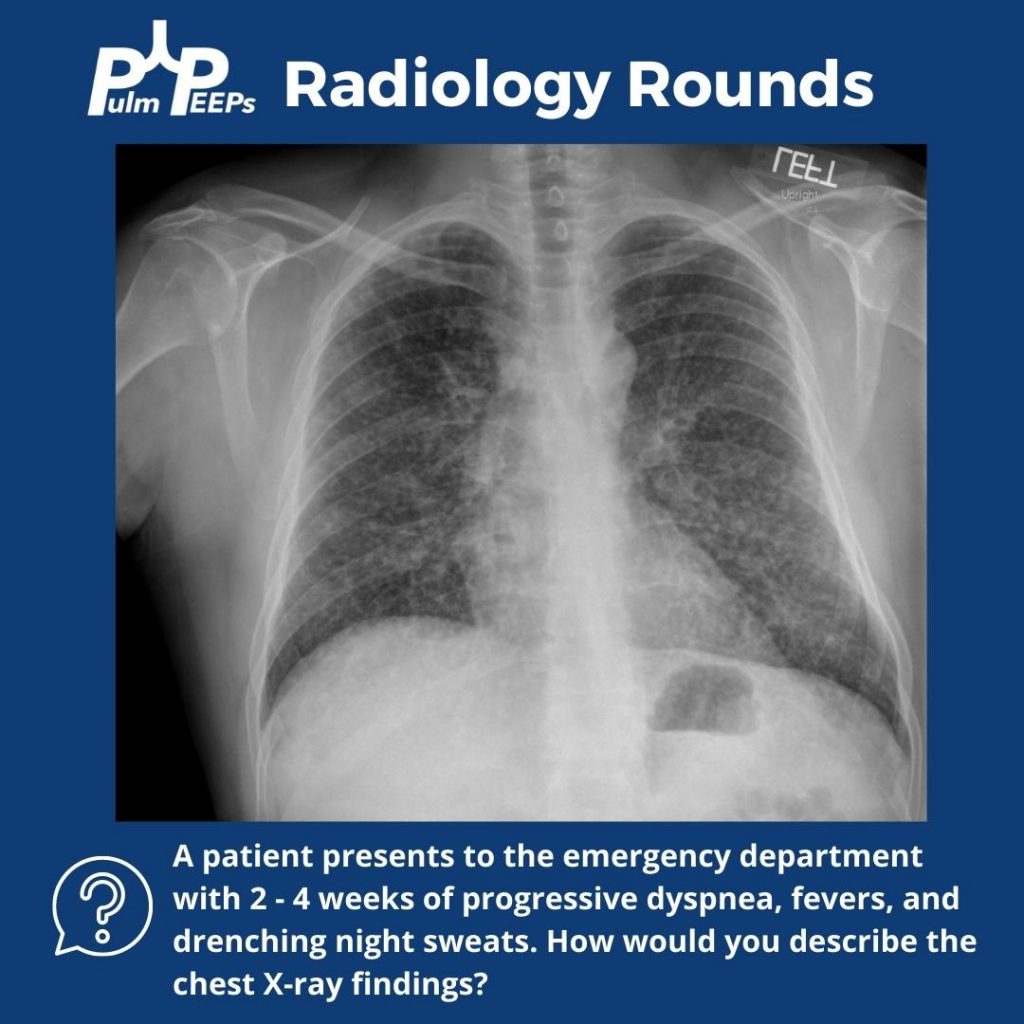
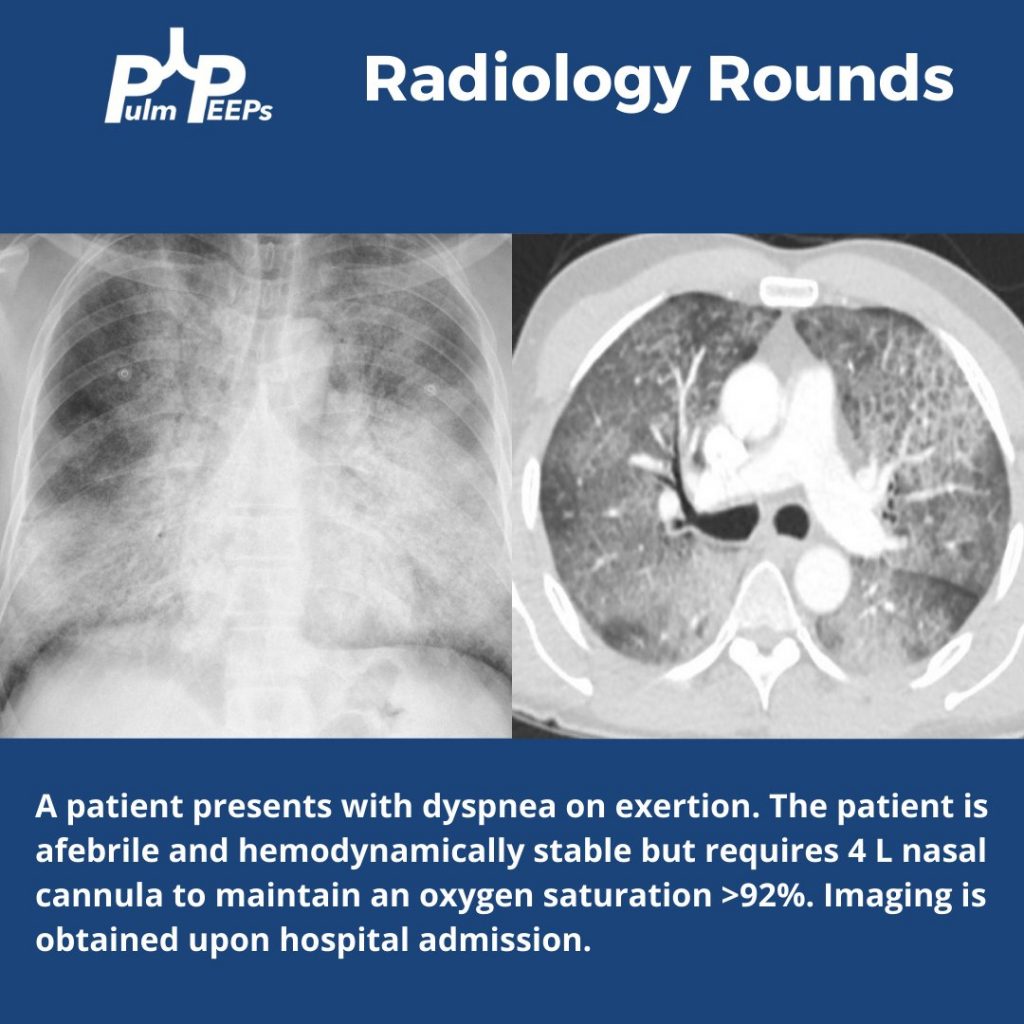
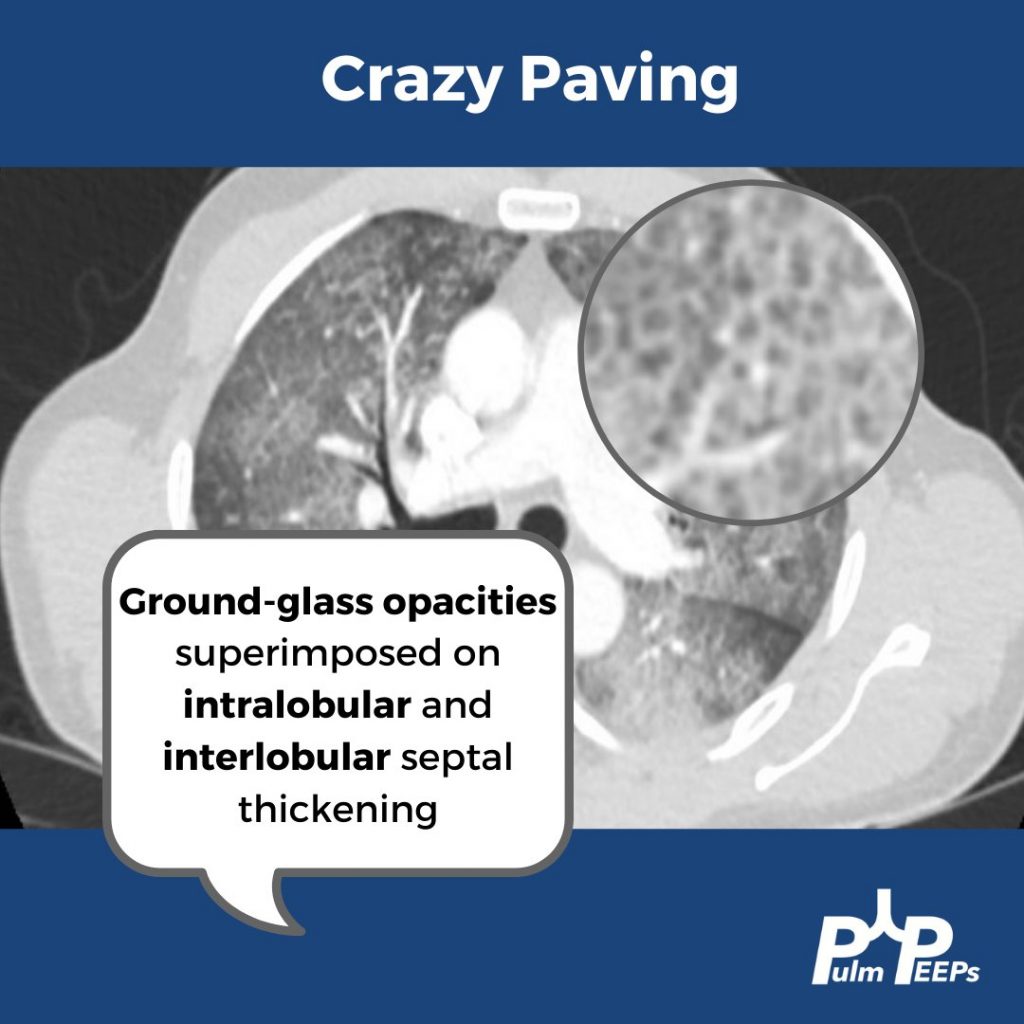
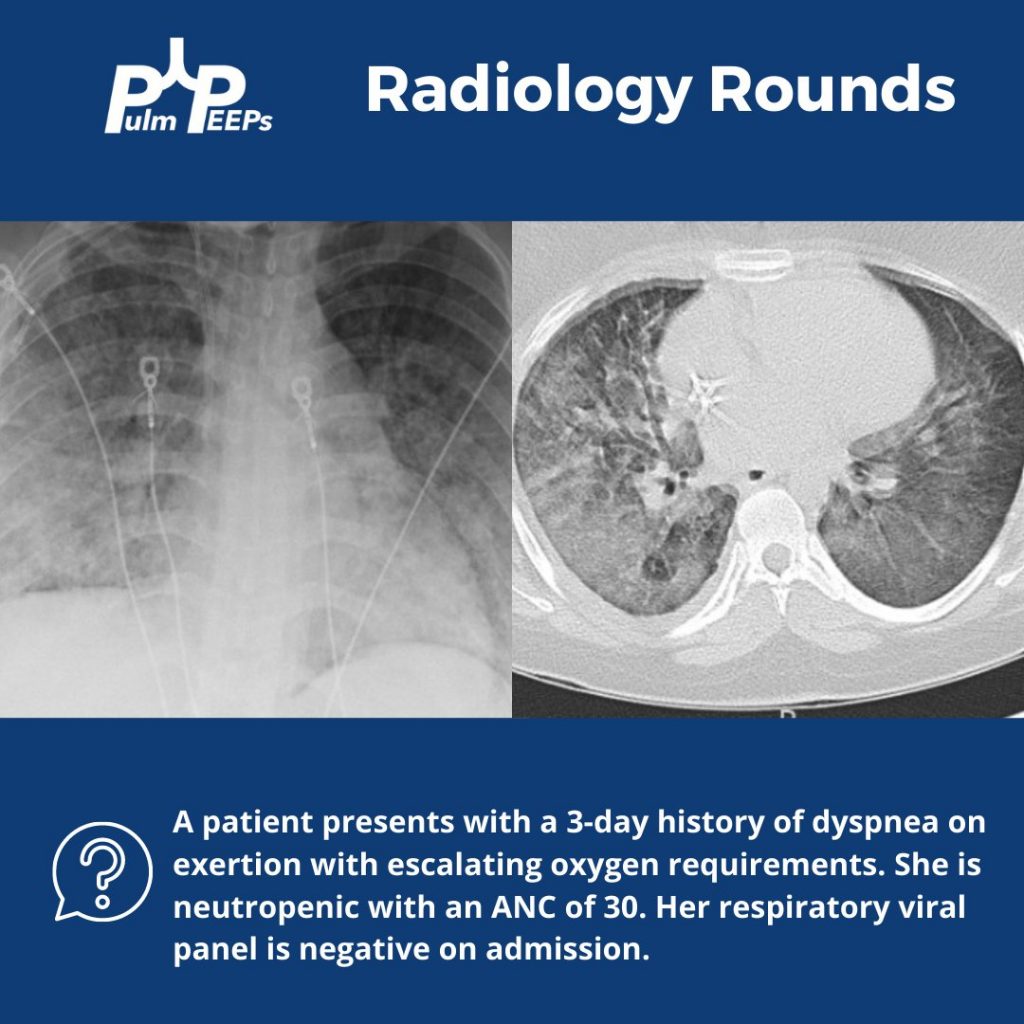
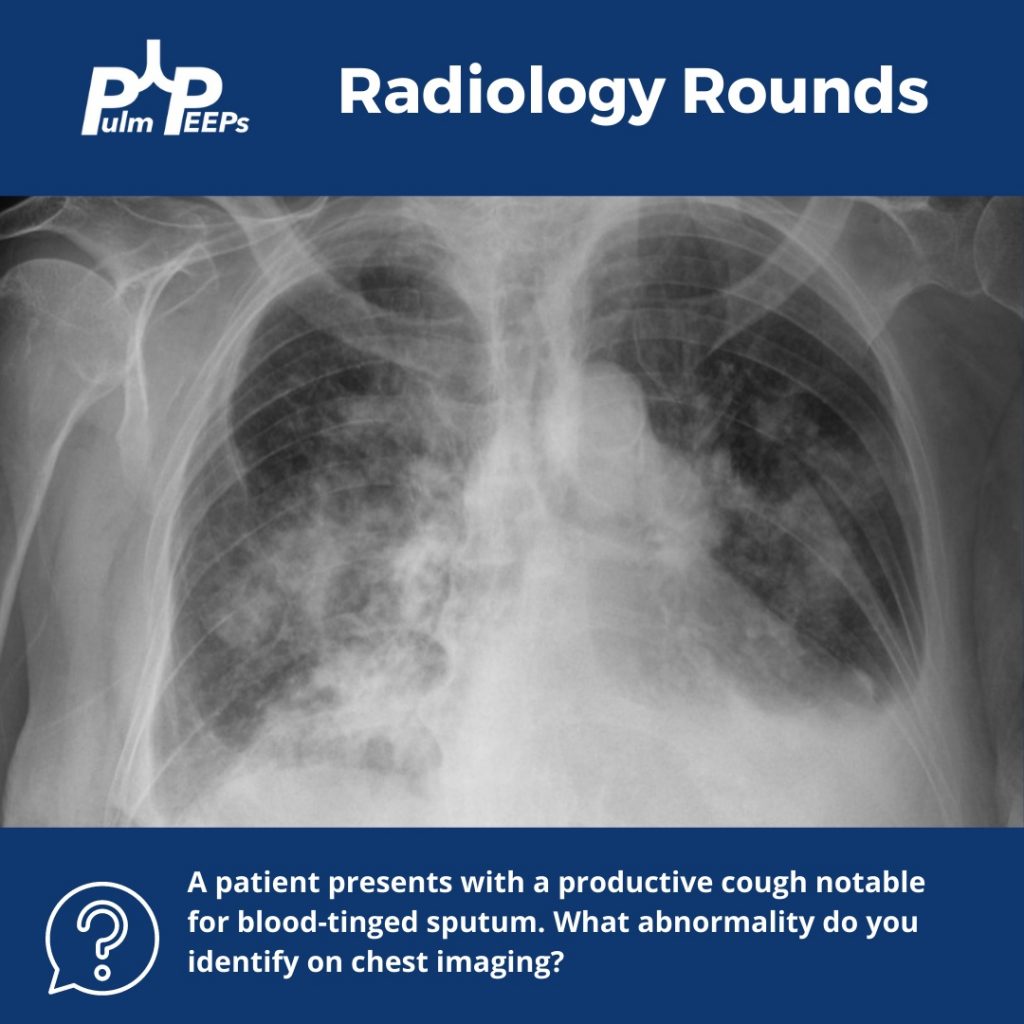
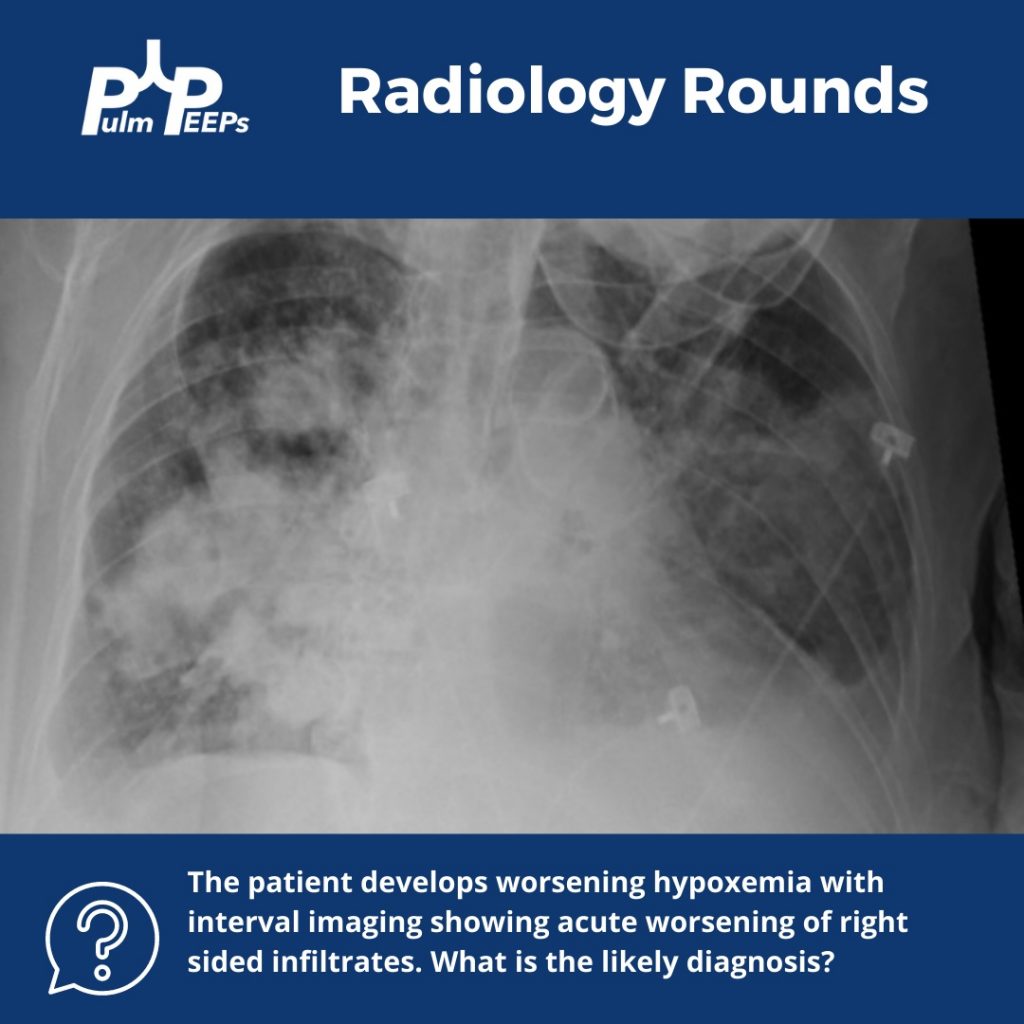
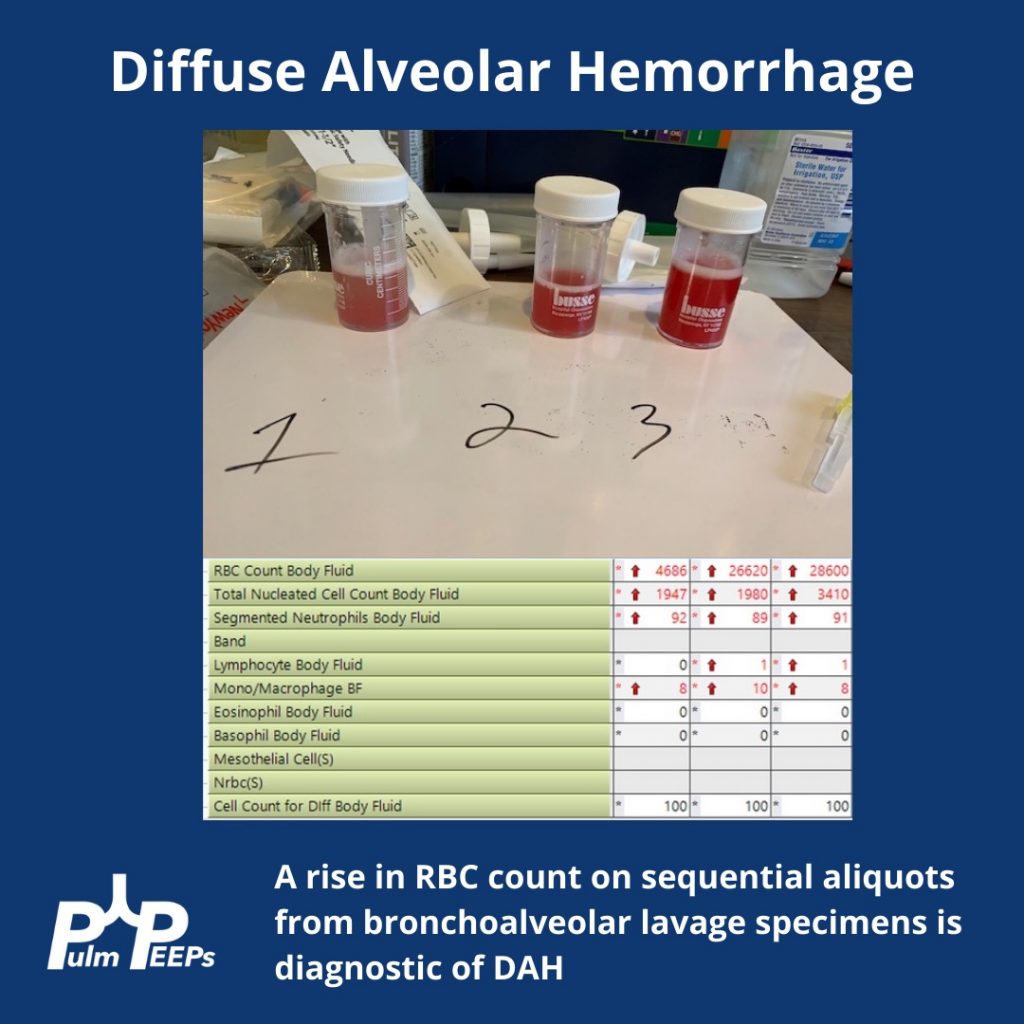
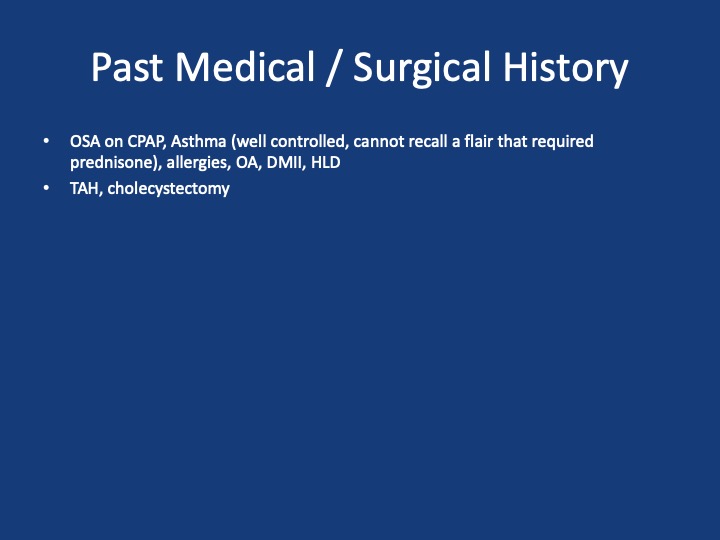
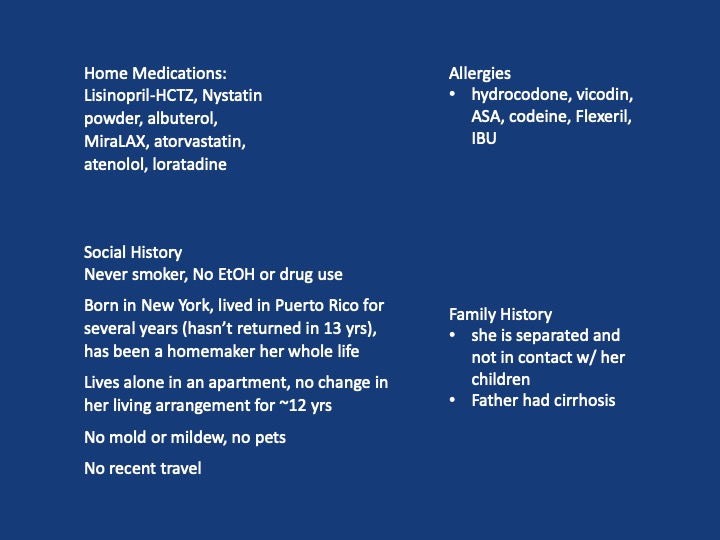
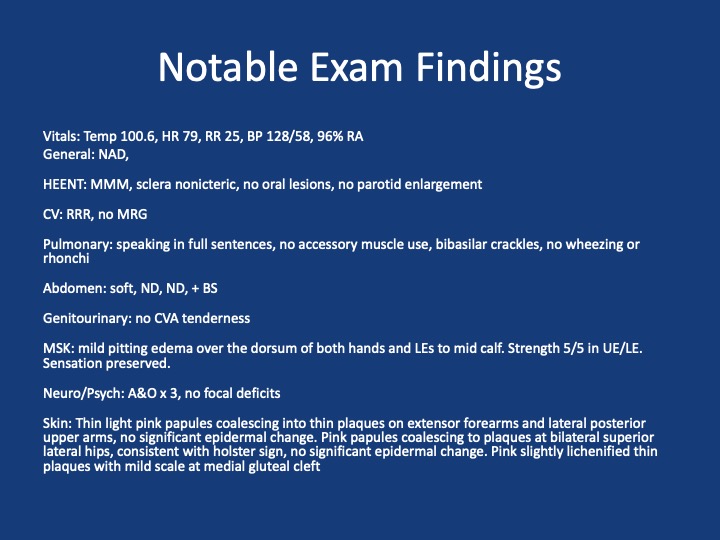
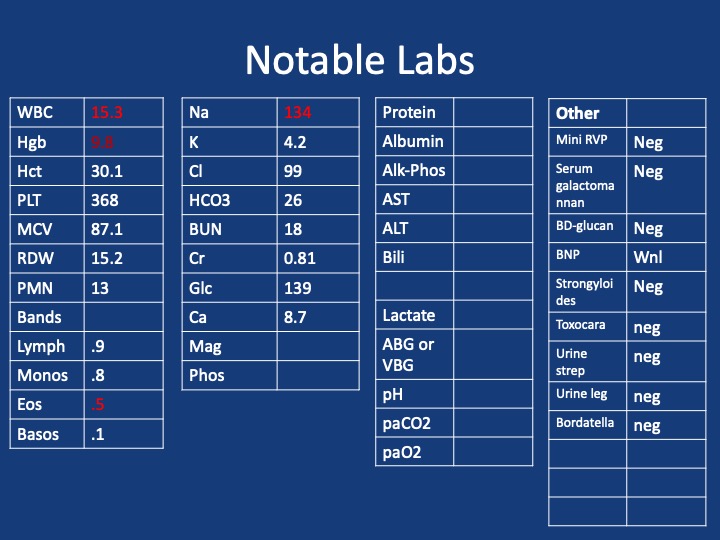
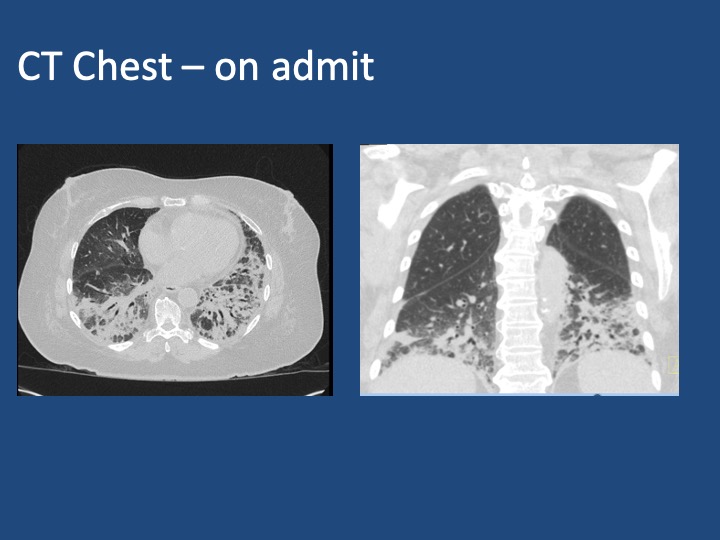
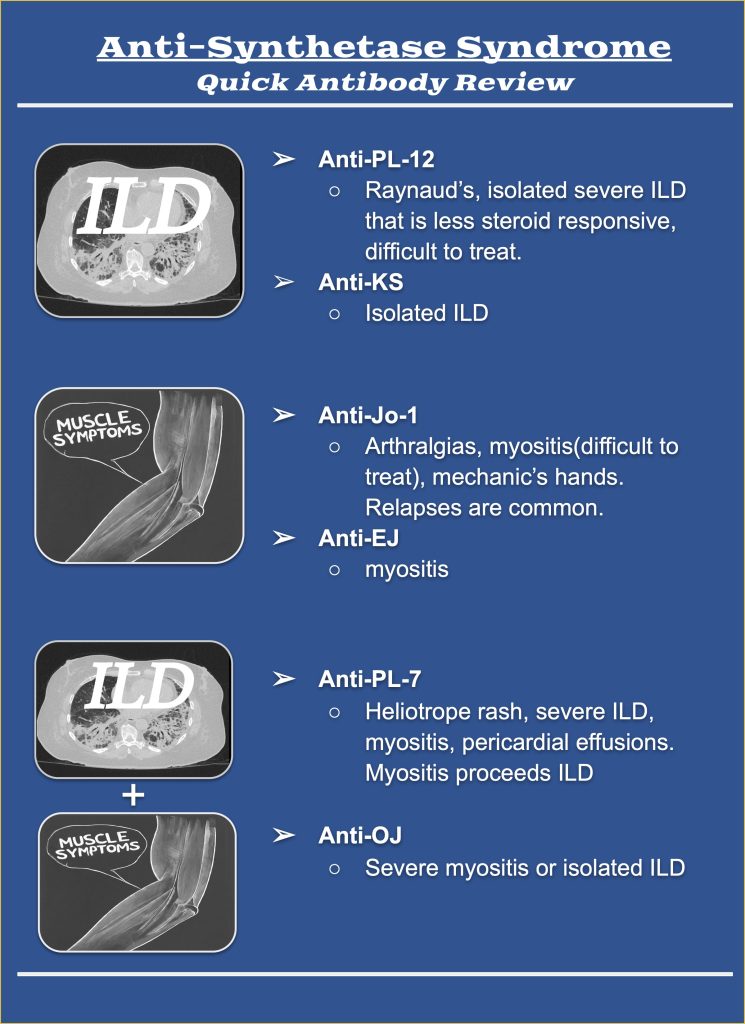
A 75 y/o F presenting with acute on chronic SOB, cough, L sided chest pain and rash. She has had ~7 months of progressive dyspnea, now a/w 2 months of productive cough, and several weeks of L sided chest pain and rash. She has been seen multiple times in the past two months for these sxs. During that time she received multiple antibiotic courses (urgent care, outpatient providers), including augmentin, azithromycin and levaquin, and asthma directed therapy (no steroids). Imaging throughout that time (CXRs, CTPE) show progression from a LLL infiltrate to bibasilar infiltrates. Despite these interventions, sxs continue to worsen. One month prior she was admitted to an OSH w/ continued worsening, vitals stable, exam nonfocal, mild leukocytosis but infectious w/u bland. Received broad spectrum abx. Bronch w/ BAL offers negative cultures, cytology, cell count w/ 66% neutrophils, 14% eosinophils. Discharged w/ dx of PNA on a 10 day course of levaquin and new exertional oxygen requirement of 2L. She then presents to Umass ~1 month later w/ continued progression of sxs
Key Learning Points
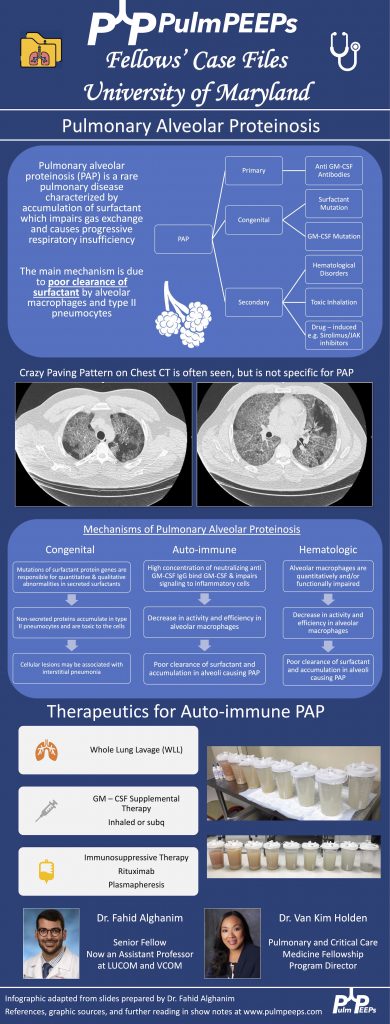
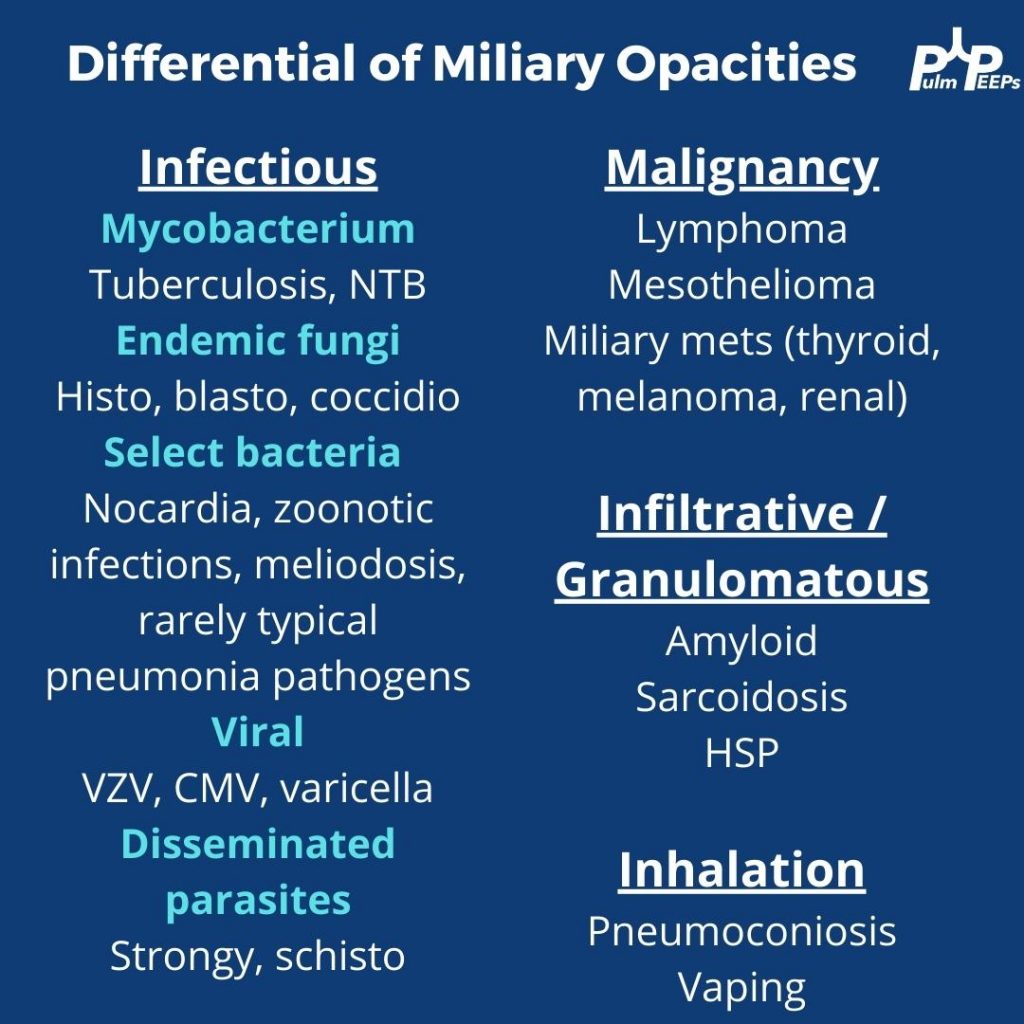
1. Formulate a differential diagnosis for non-resolving pneumonia
2. Evaluate the utility of transbronchial biopsy in the workup of undifferentiated ILD
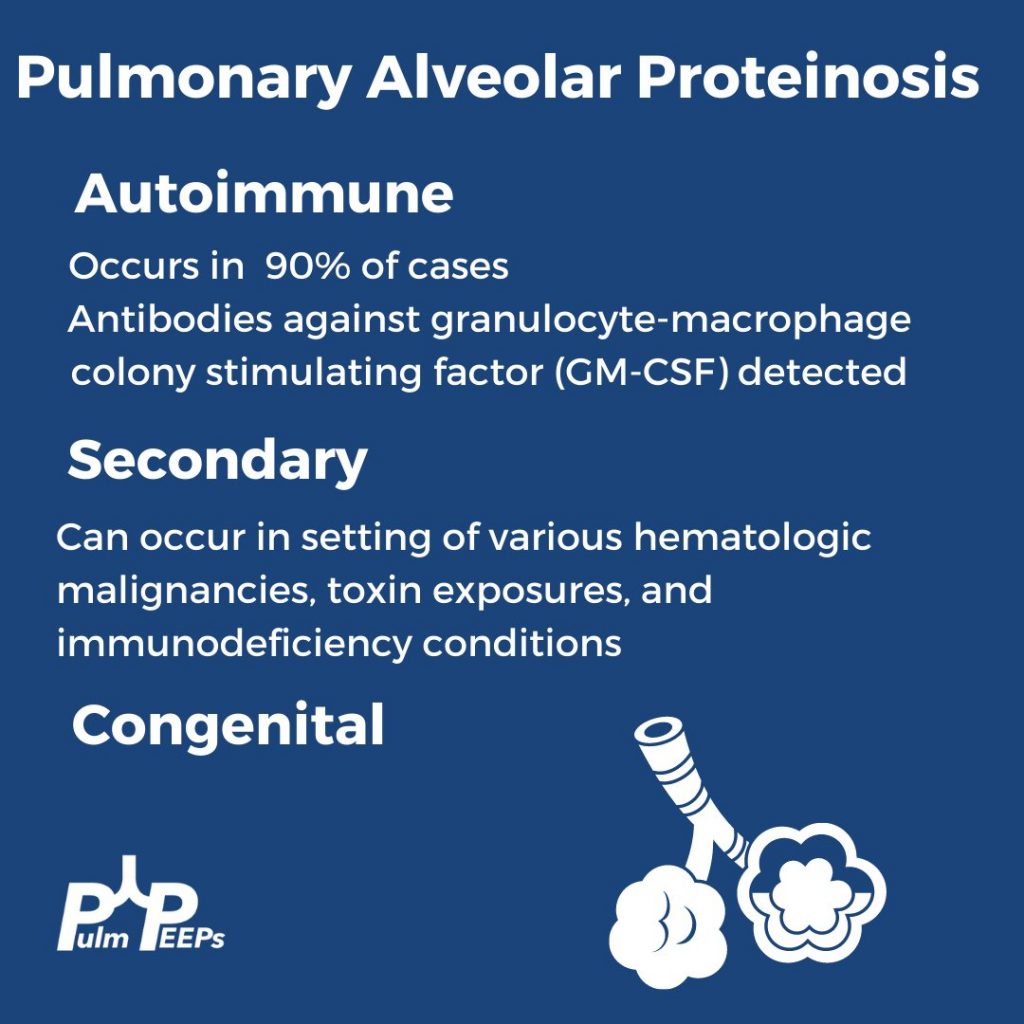
3. Describe the clinical manifestations of antisynthetase syndrome and identify the differences in presentation associated with PL-12 positivity
References and Further Reading
1. Kuru T, Lynch JP 3rd. Nonresolving or slowly resolving pneumonia. Clin Chest Med. 1999 Sep;20(3):623-51. doi: 10.1016/s0272-5231(05)70241-0. PMID: 10516909.
2. Troy LK, Grainge C, Corte TJ, Williamson JP, Vallely MP, Cooper WA, Mahar A, Myers JL, Lai S, Mulyadi E, Torzillo PJ, Phillips MJ, Jo HE, Webster SE, Lin QT, Rhodes JE, Salamonsen M, Wrobel JP, Harris B, Don G, Wu PJC, Ng BJ, Oldmeadow C, Raghu G, Lau EMT; Cryobiopsy versus Open Lung biopsy in the Diagnosis of Interstitial lung disease alliance (COLDICE) Investigators. Diagnostic accuracy of transbronchial lung cryobiopsy for interstitial lung disease diagnosis (COLDICE): a prospective, comparative study. Lancet Respir Med. 2020 Feb;8(2):171-181. doi: 10.1016/S2213-2600(19)30342-X. Epub 2019 Sep 29. PMID: 31578168.
3. Hallowell RW, Danoff SK. Diagnosis and Management of Myositis-Associated Lung Disease. Chest. 2023 Jun;163(6):1476-1491. doi: 10.1016/j.chest.2023.01.031. Epub 2023 Feb 9. PMID: 36764512.
4. Hallowell RW, Paik JJ. Myositis-associated interstitial lung disease: a comprehensive approach to diagnosis and management. Clin Exp Rheumatol. 2022 Feb;40(2):373-383. doi: 10.55563/clinexprheumatol/brvl1v. Epub 2021 Mar 25. PMID: 33769263; PMCID: PMC8855729.
5. Marie I, Josse S, Decaux O, Dominique S, Diot E, Landron C, Roblot P, Jouneau S, Hatron PY, Tiev KP, Vittecoq O, Noel D, Mouthon L, Menard JF, Jouen F. Comparison of long-term outcome between anti-Jo1- and anti-PL7/PL12 positive patients with antisynthetase syndrome. Autoimmun Rev. 2012 Aug;11(10):739-45. doi: 10.1016/j.autrev.2012.01.006. Epub 2012 Feb 3. PMID: 22326685.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More