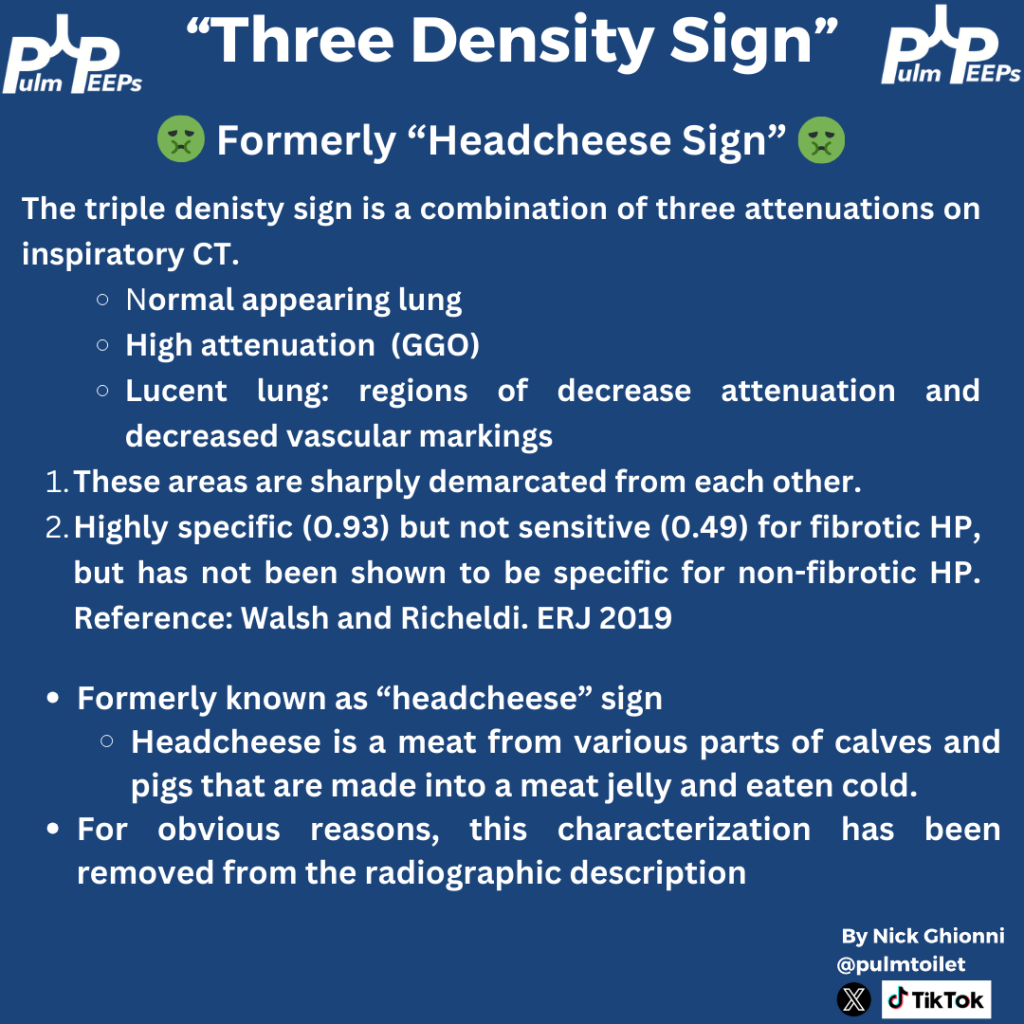
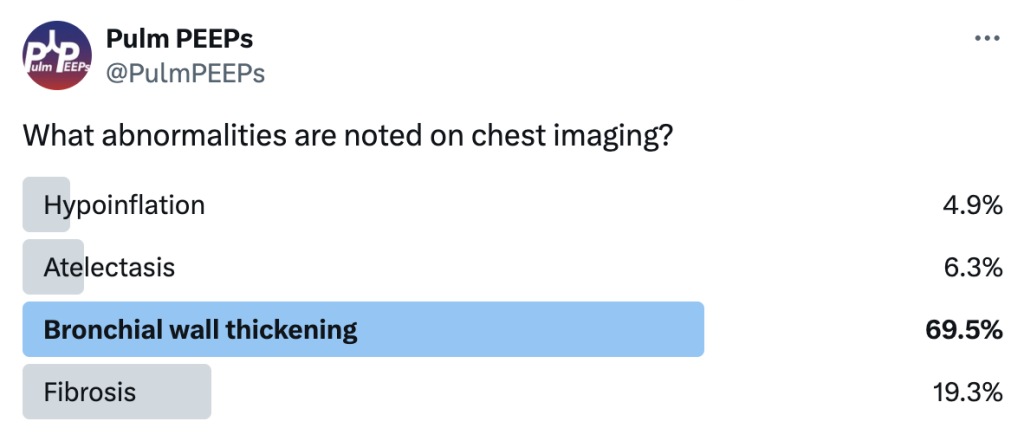
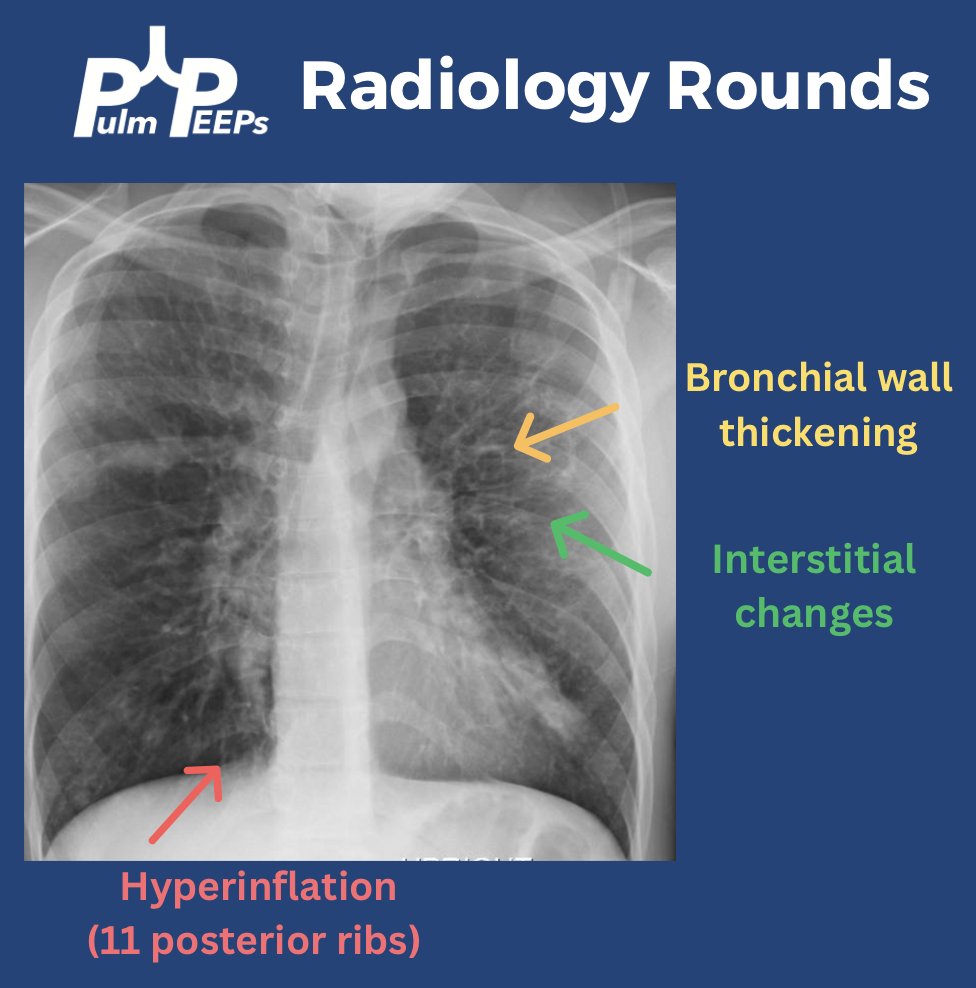
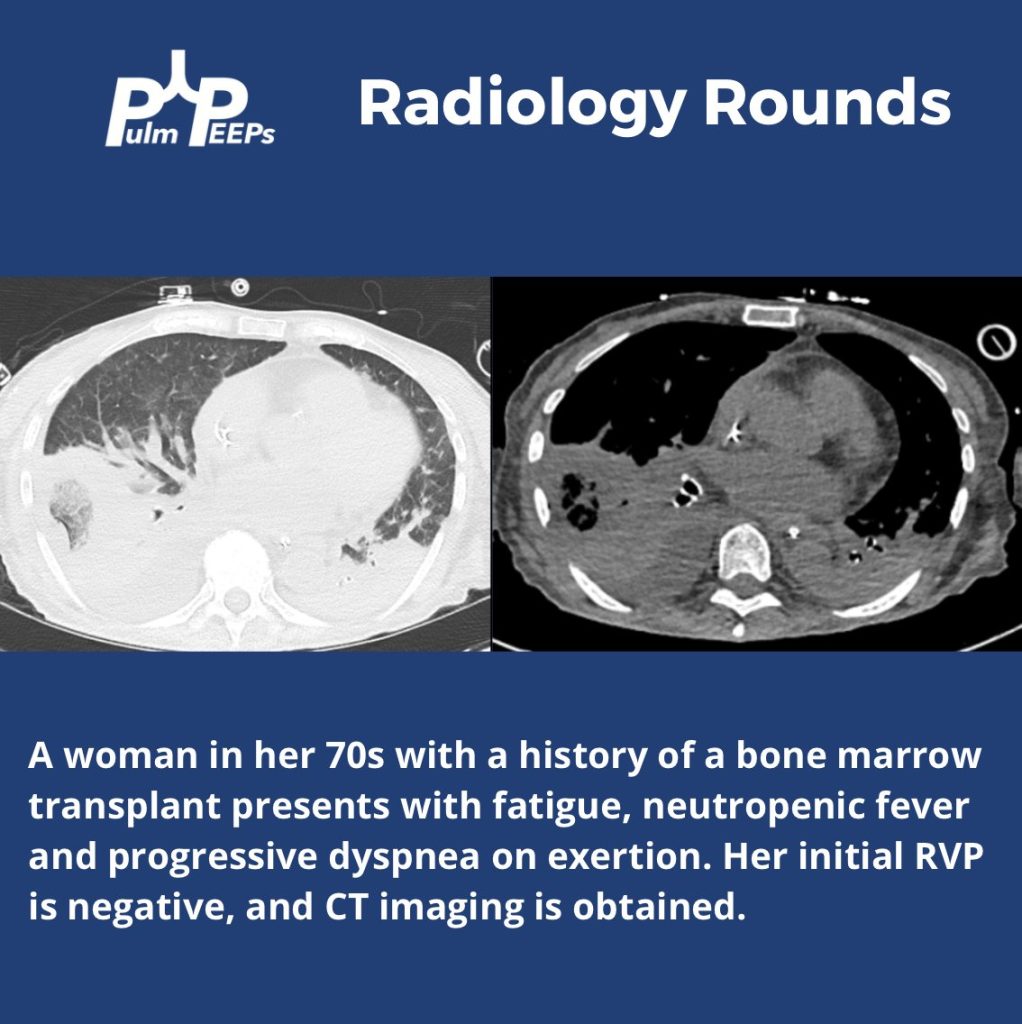
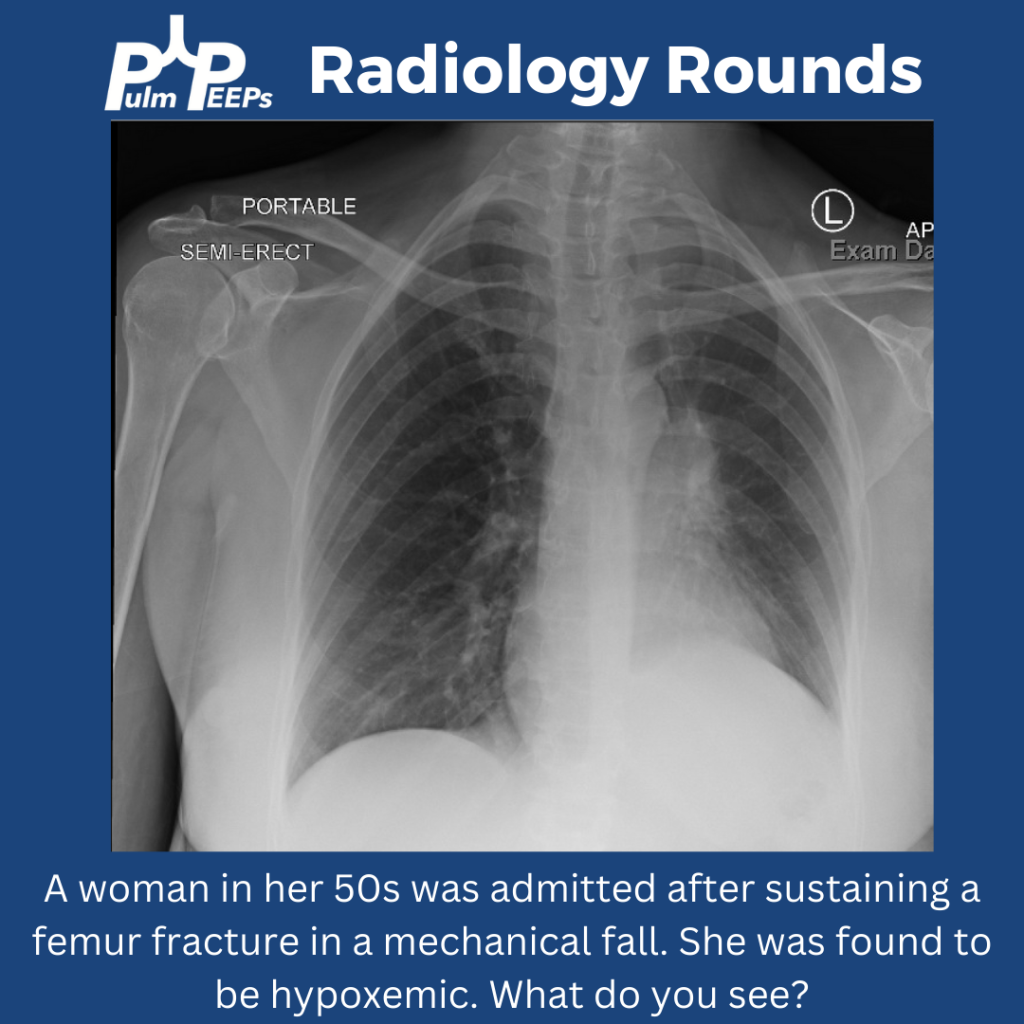
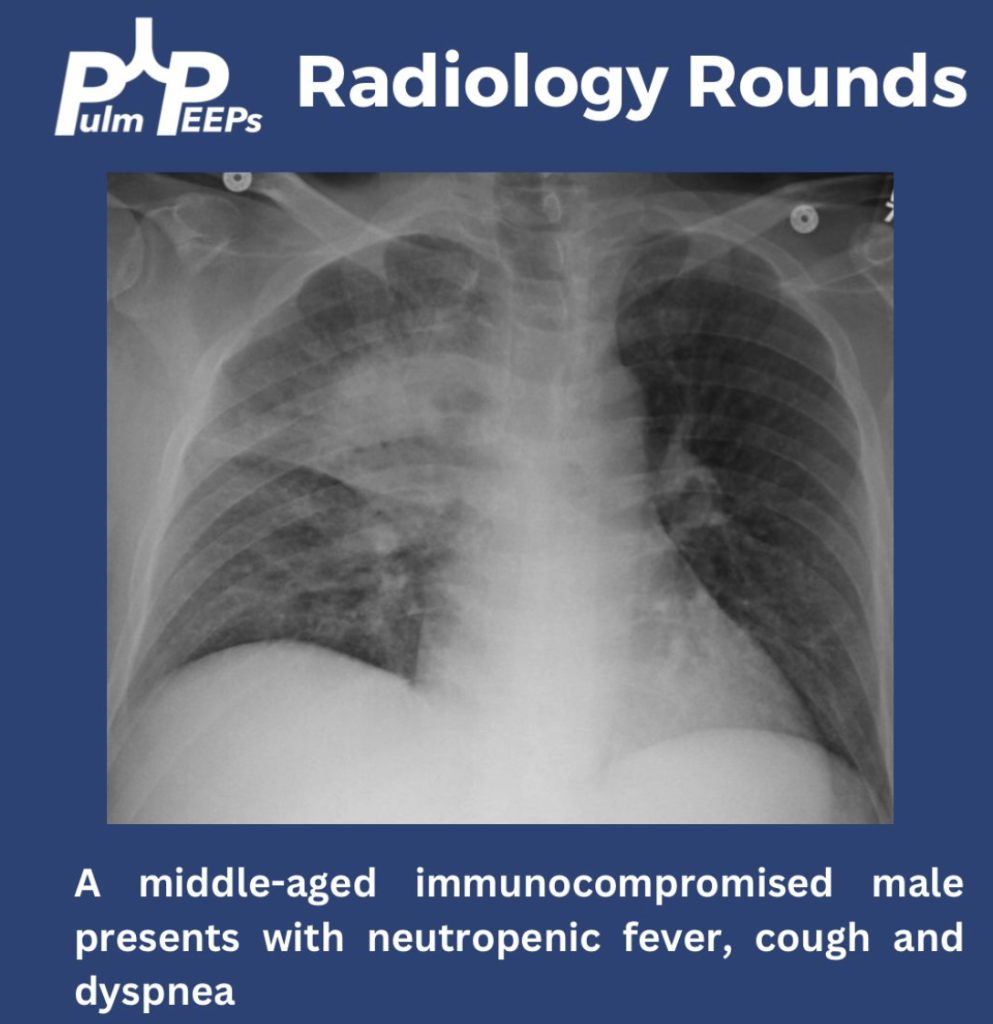
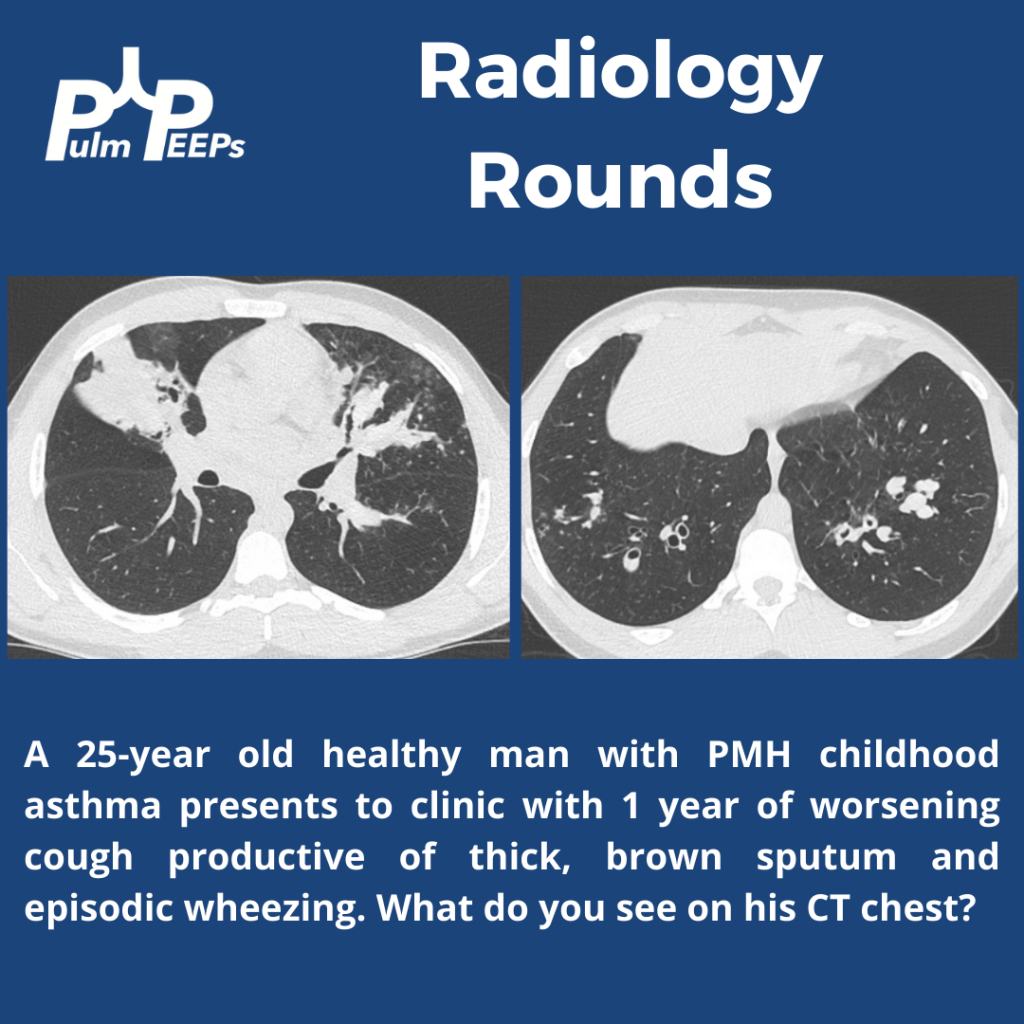
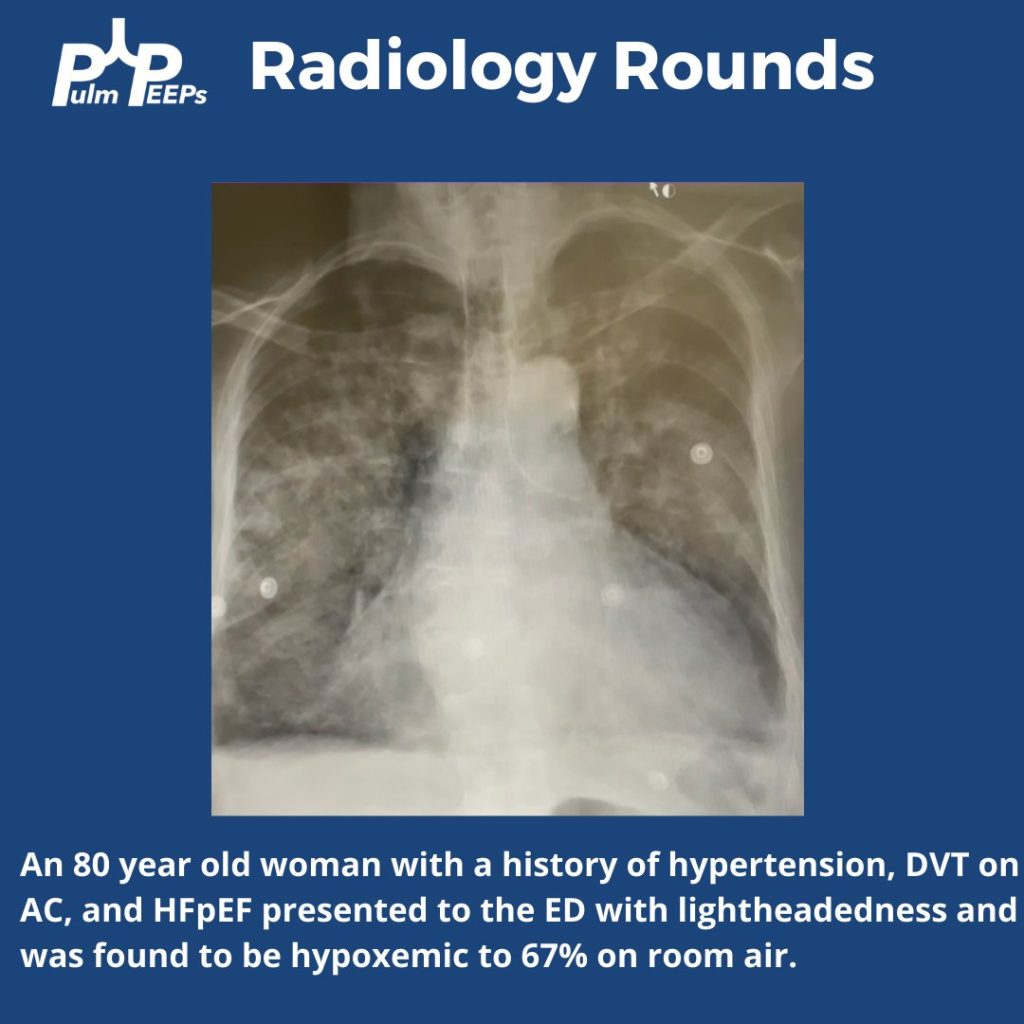
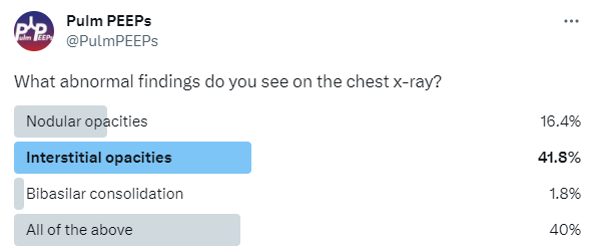
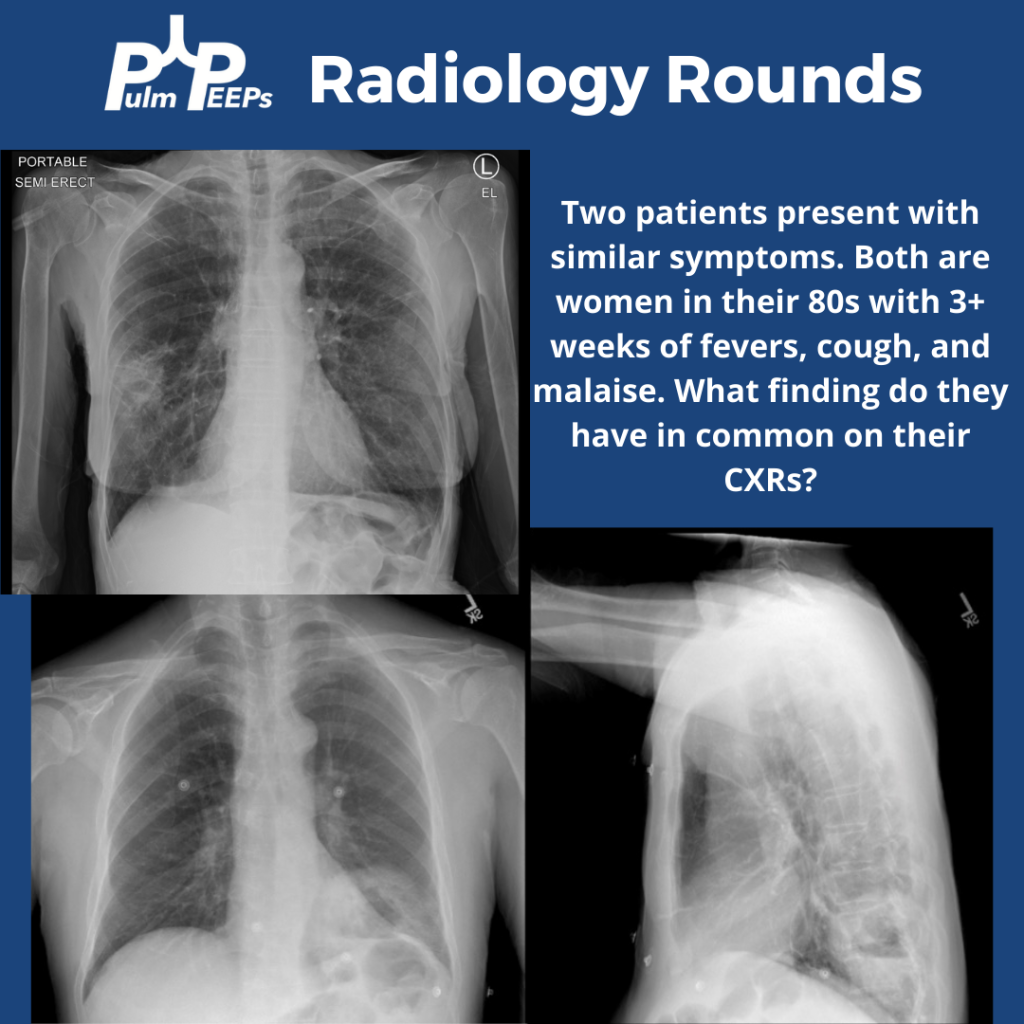
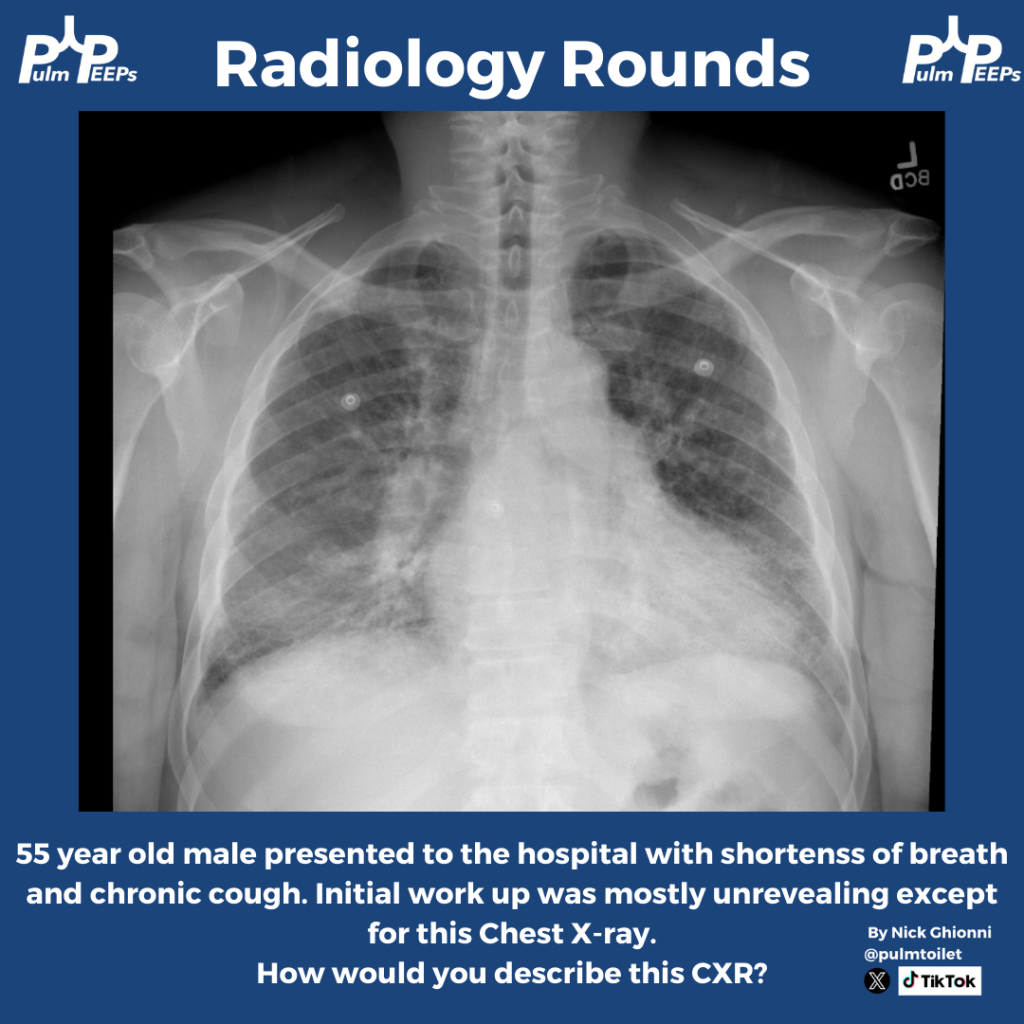
Time for another Radiology Rounds! This case is brought to you by our Associate Editor Nick Ghionni @pulmtoilet ! A 55 year old man presents to the hospital with progressive dyspnea and a chronic cough. Here is his initial CXR.
Further history and exam is taken and is notable for
Progressive dyspnea, especially with exertion
Has received courses of steroids and antibiotics in the past
Breeds pigeons
Tachypneic on exam, scattered rales, and rare faint wheeze
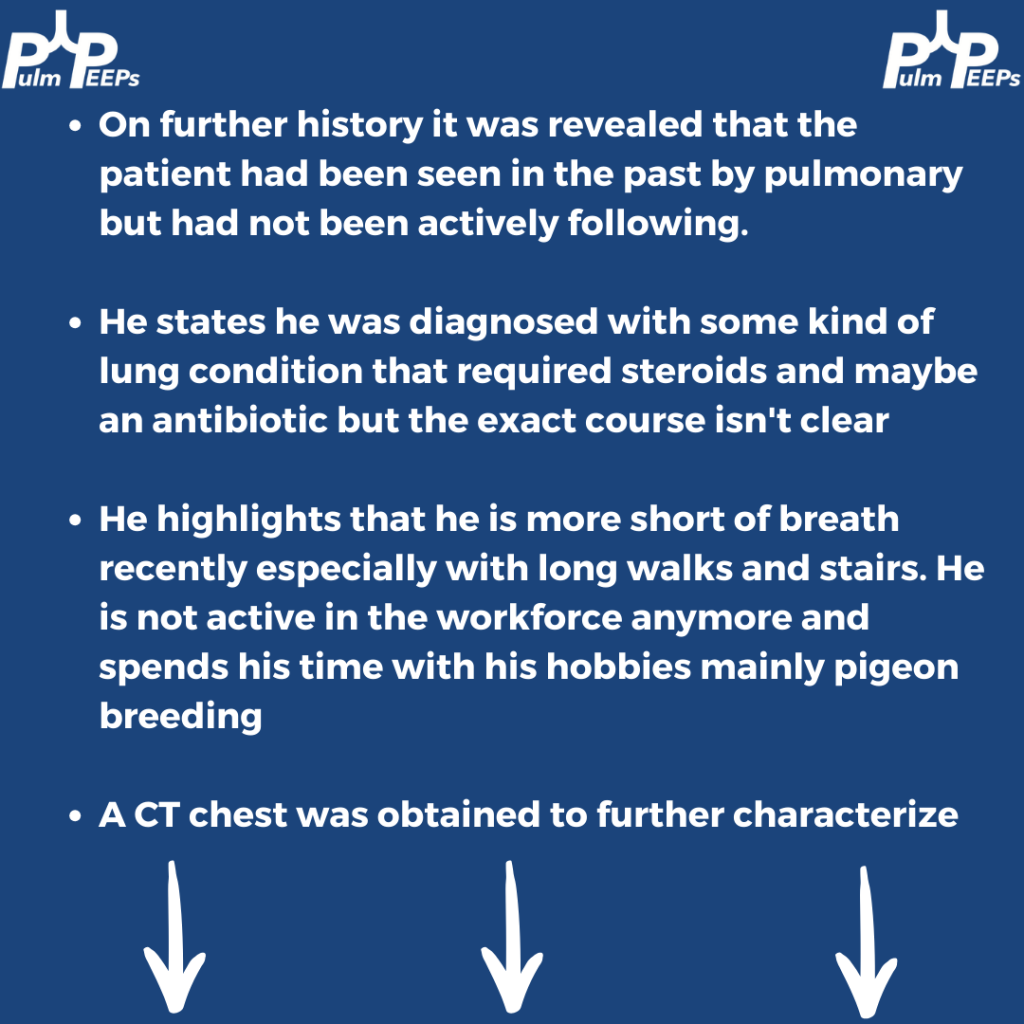

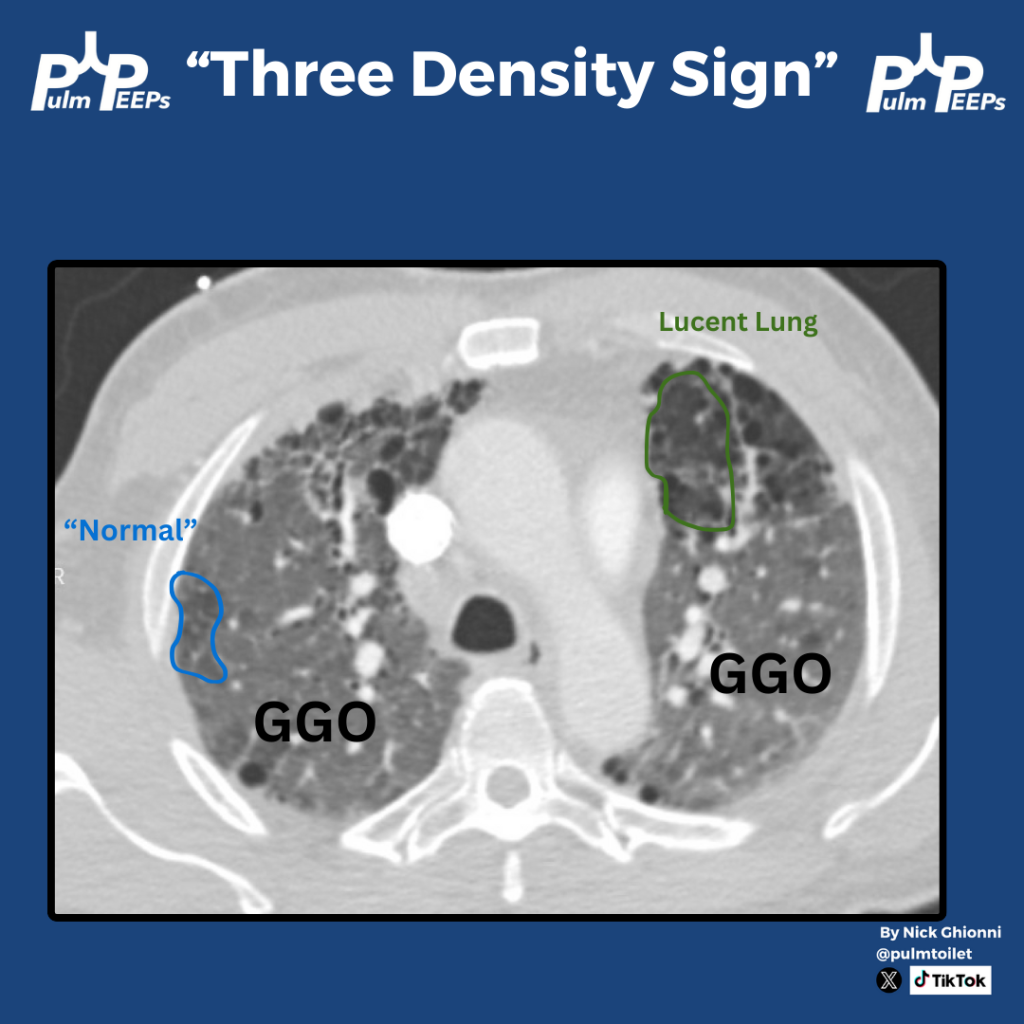
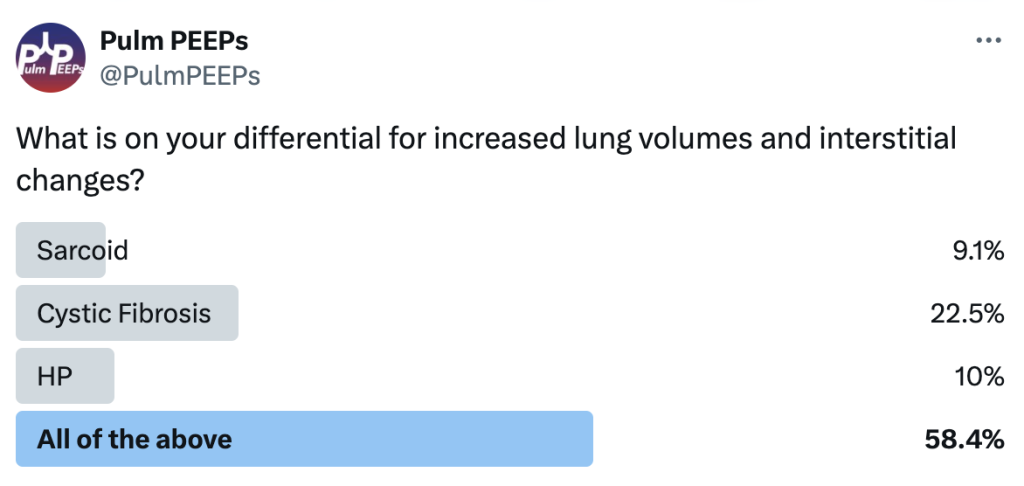
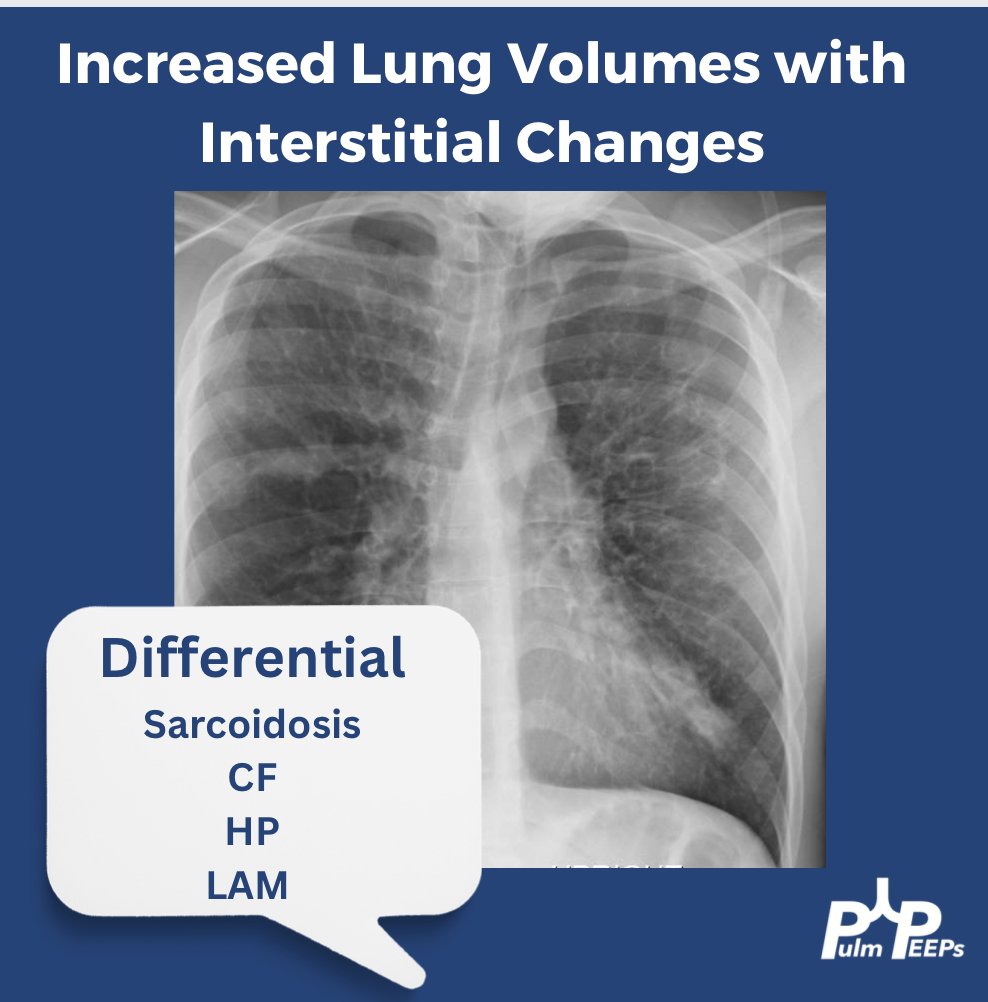
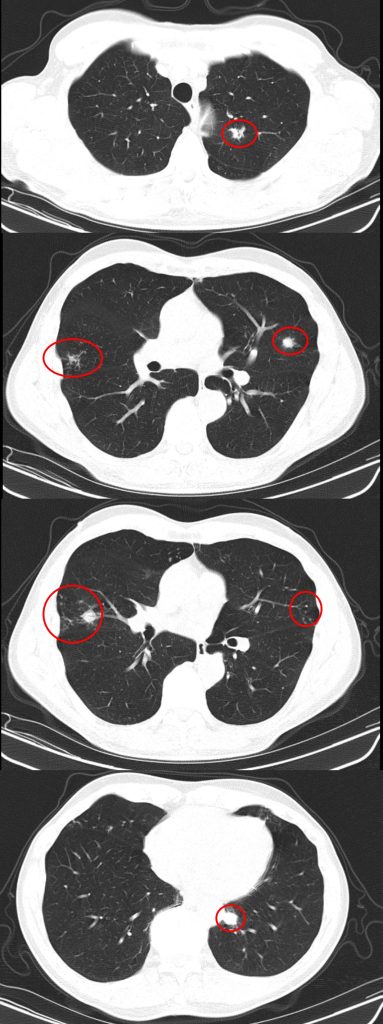
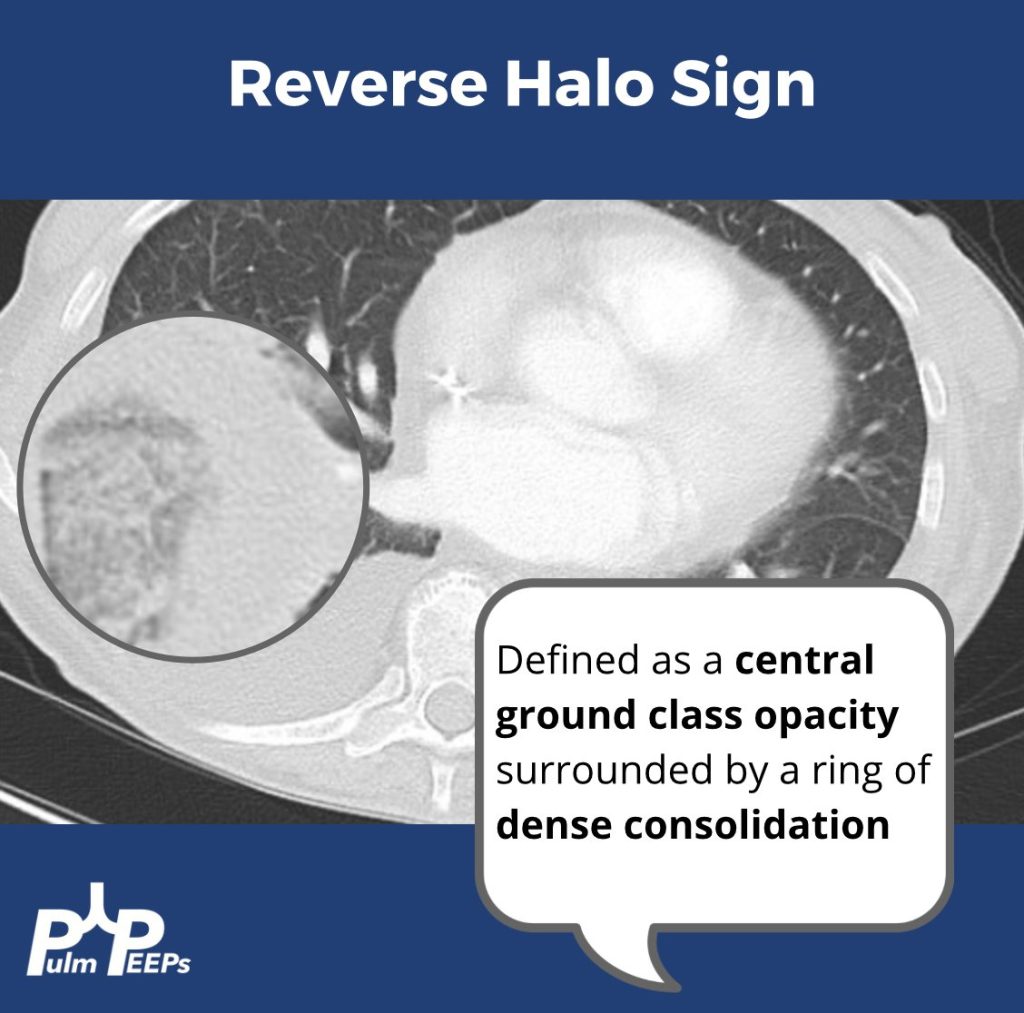
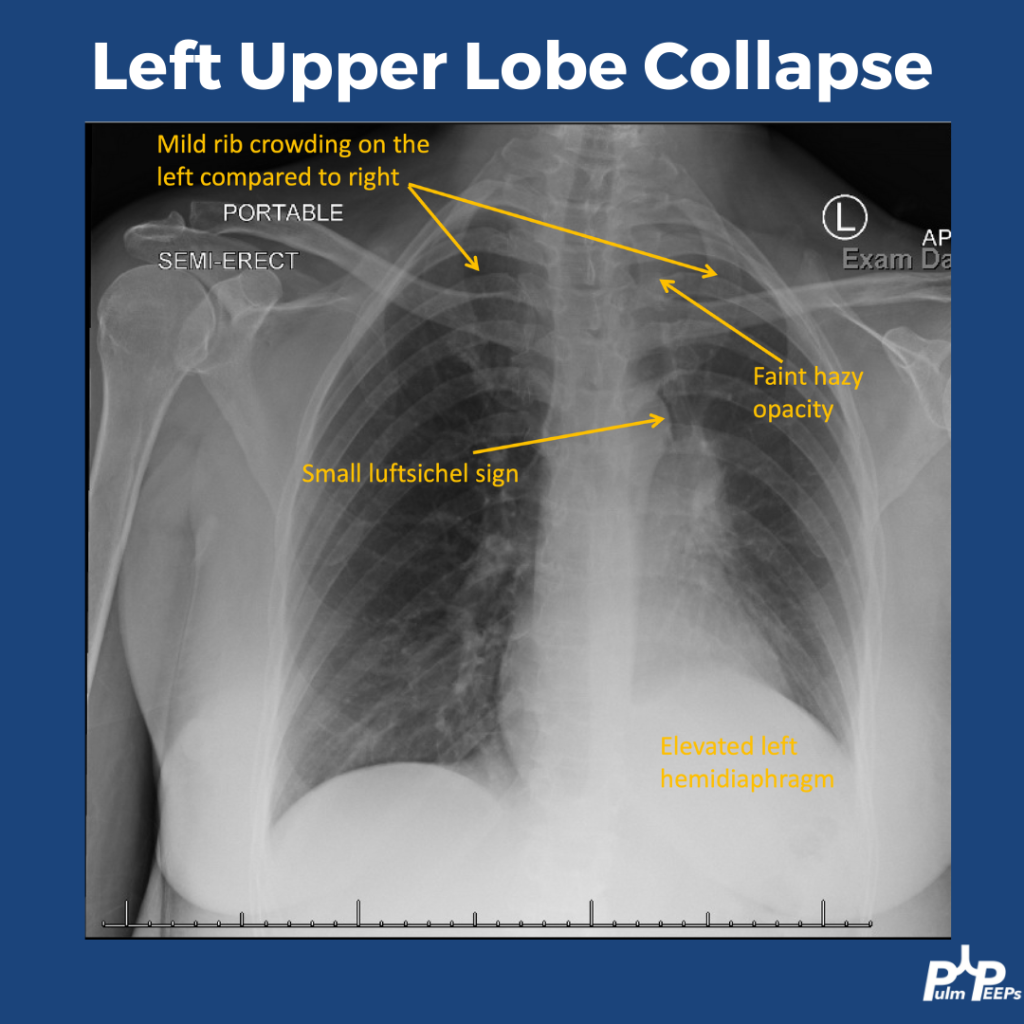
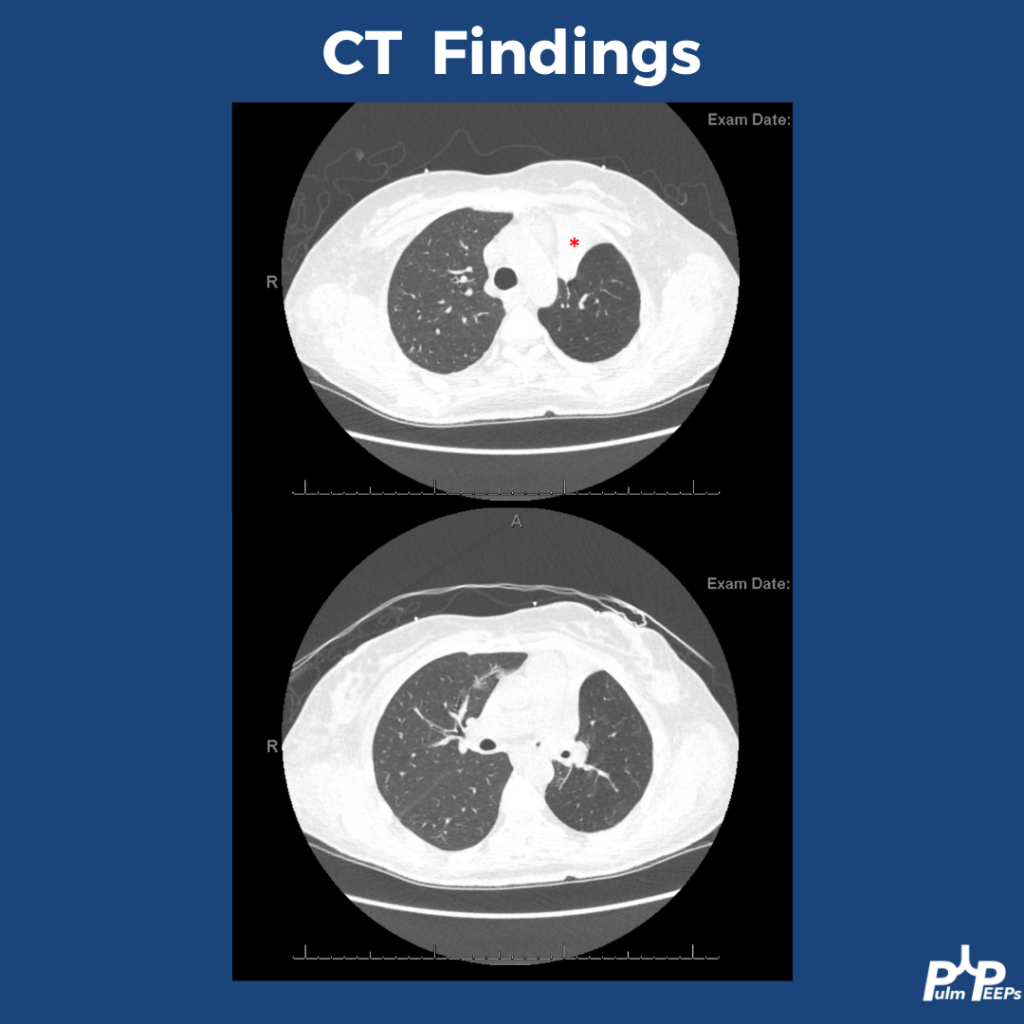
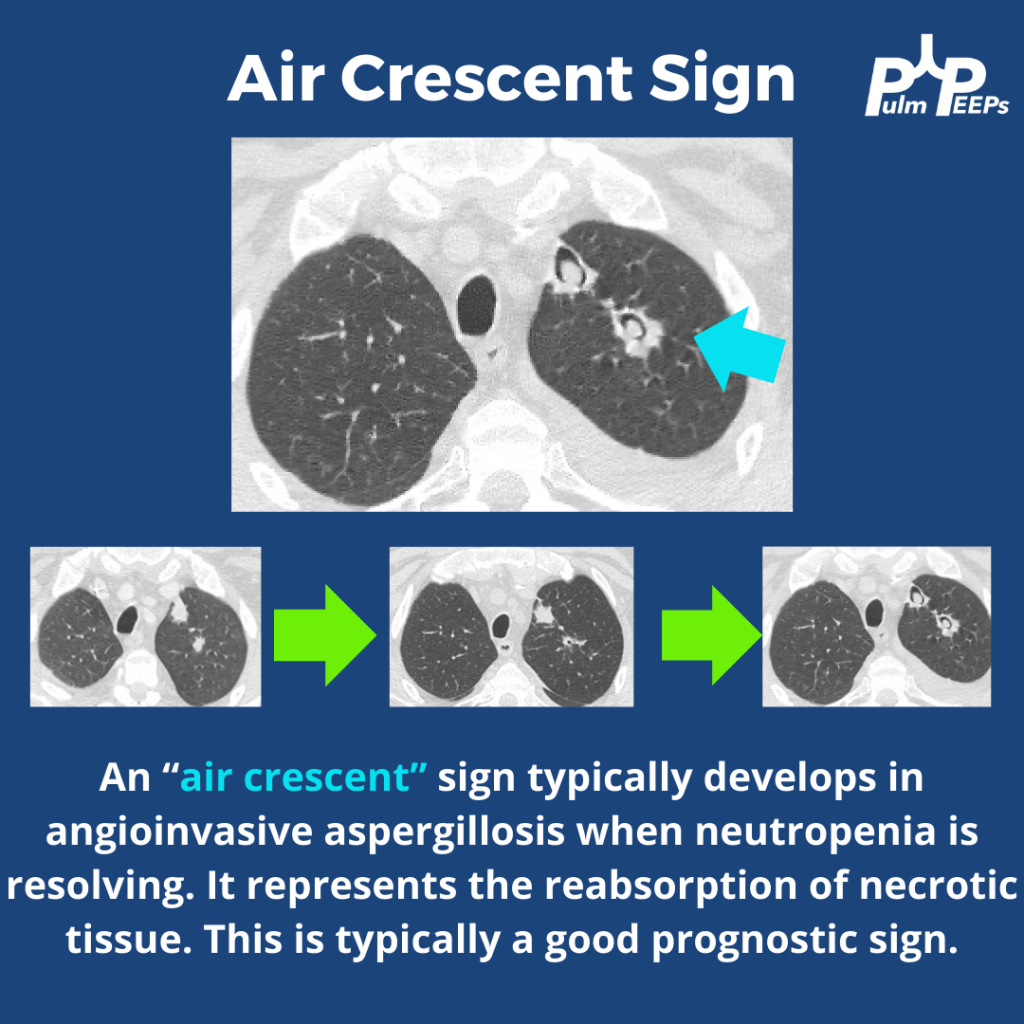
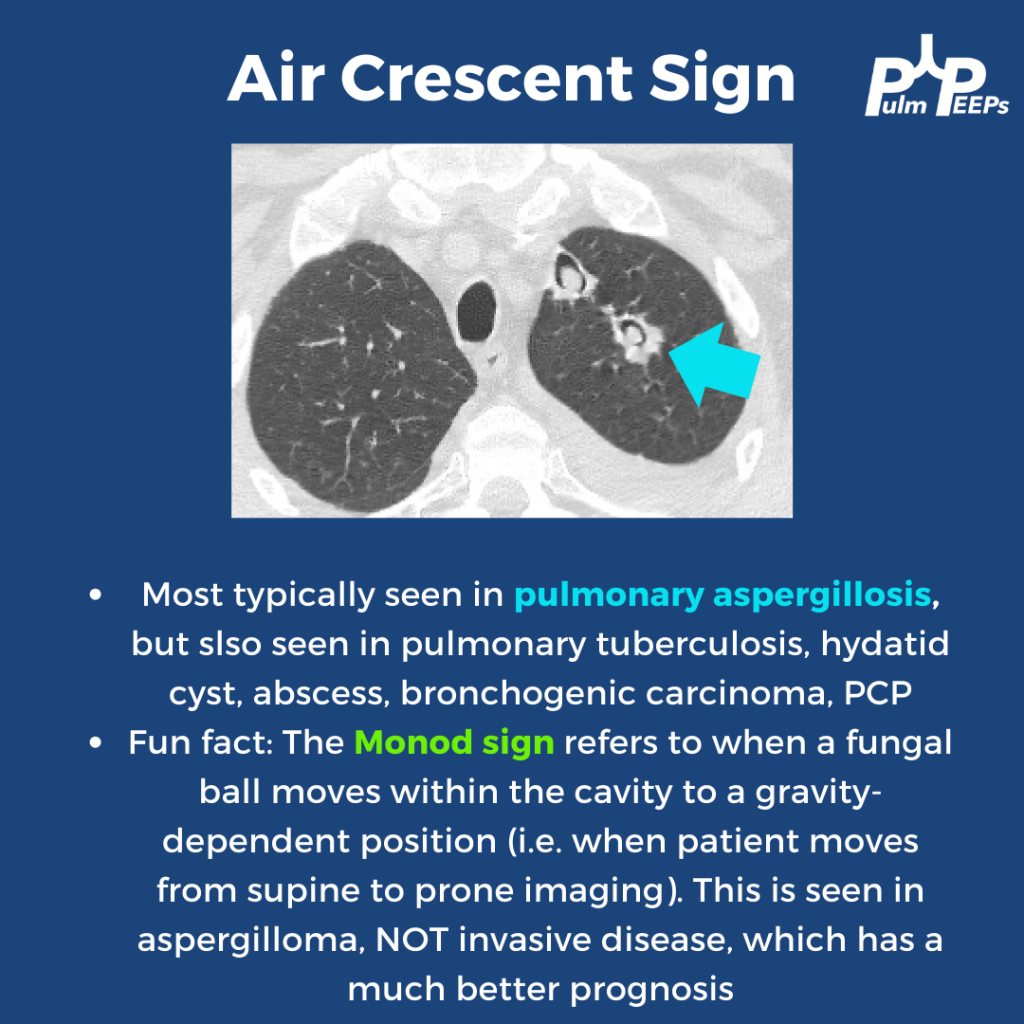
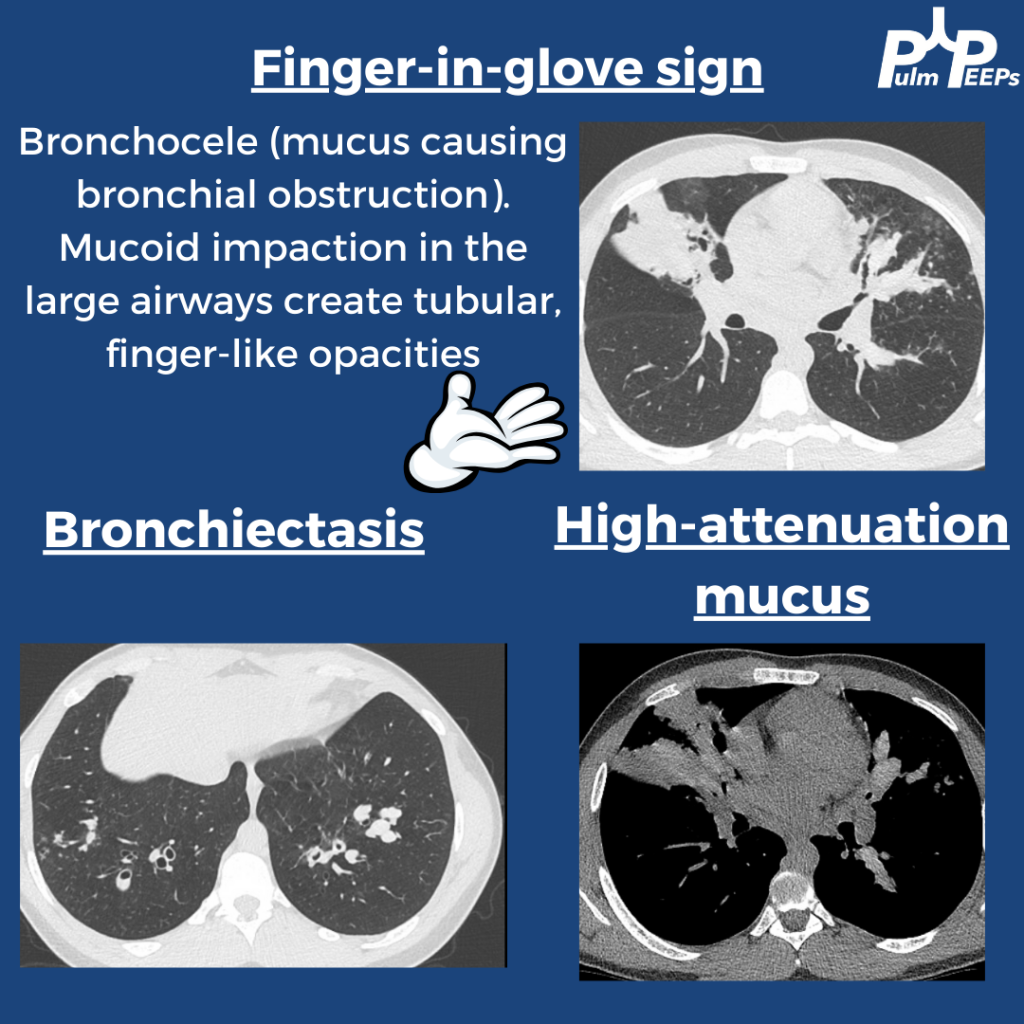
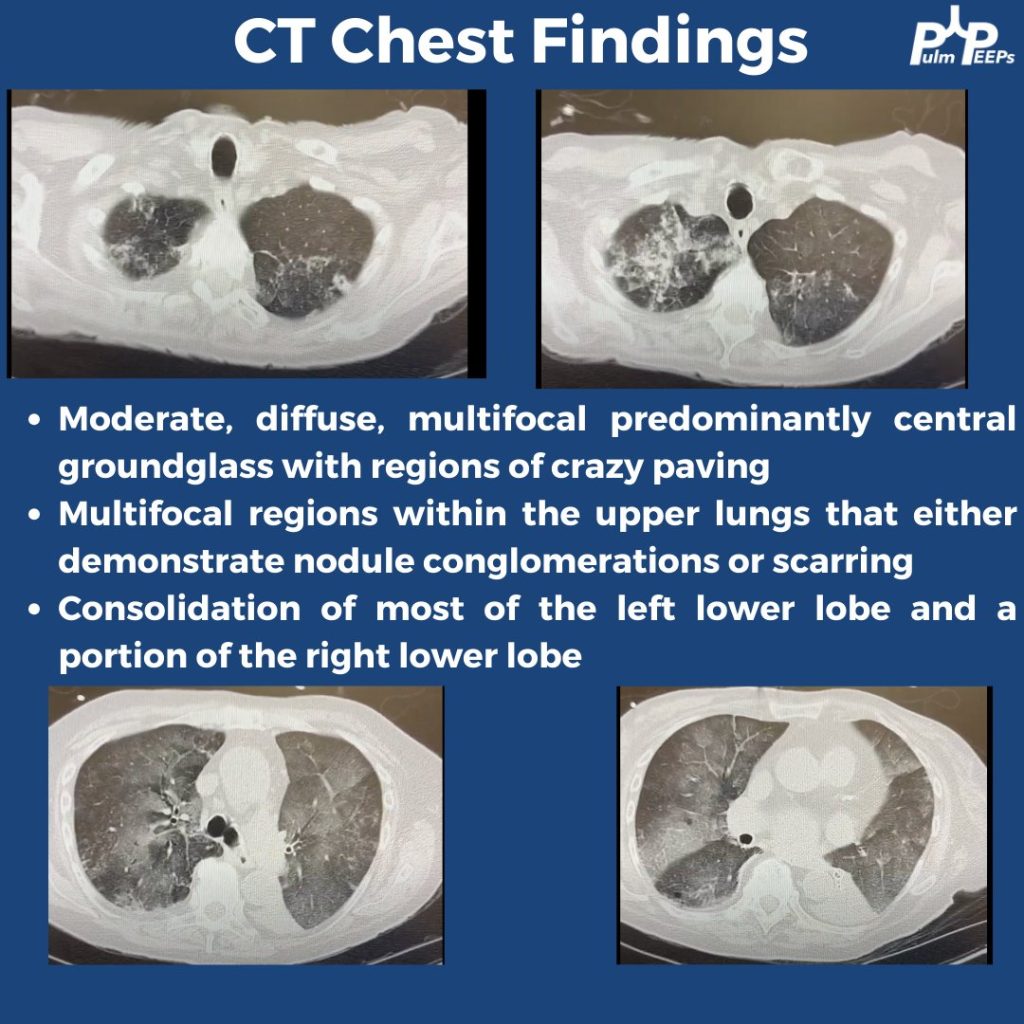
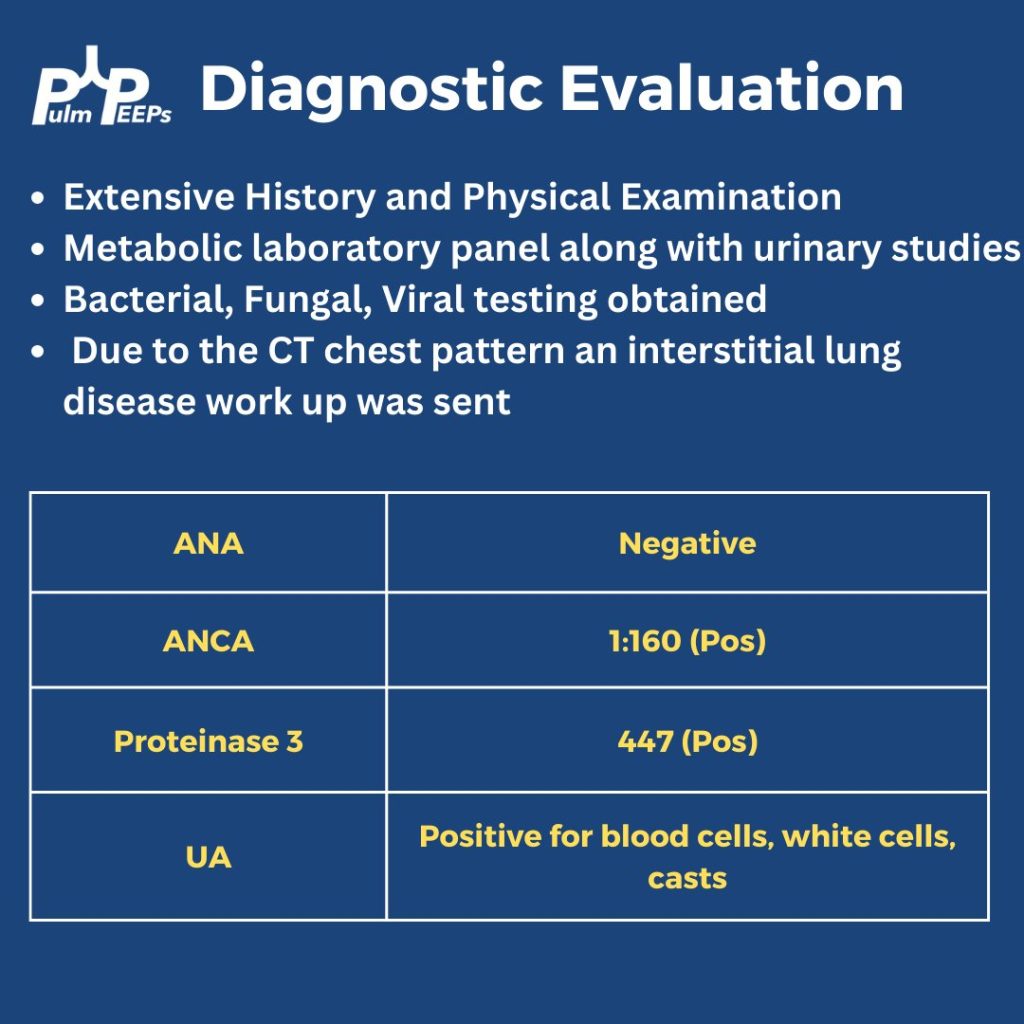
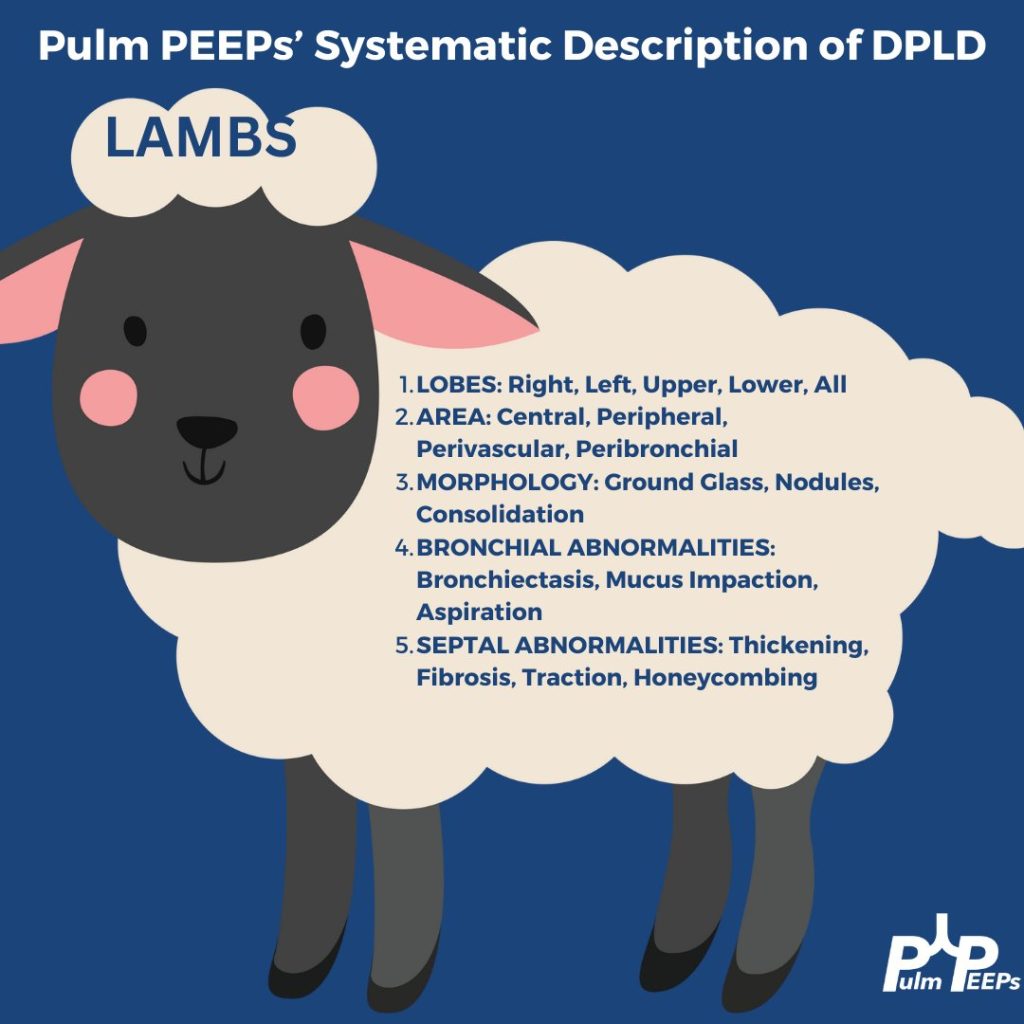
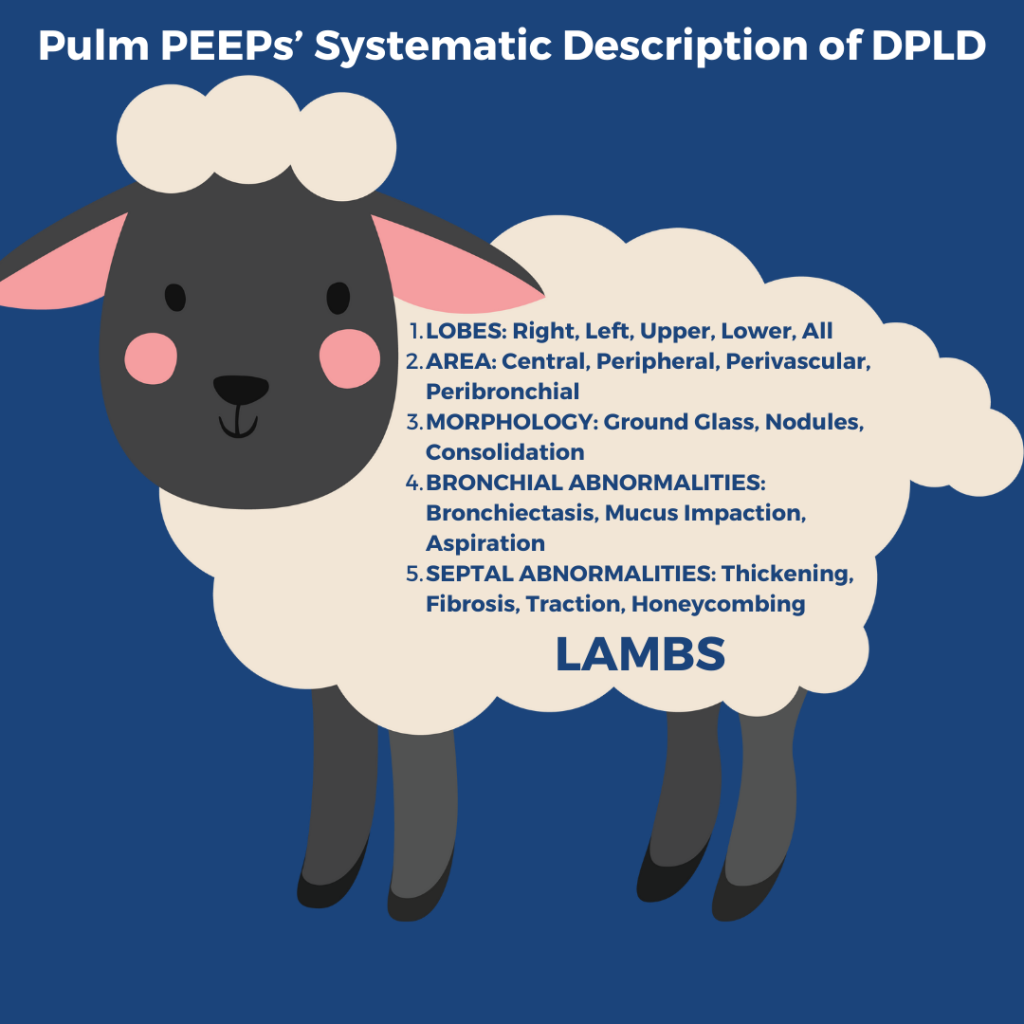
A high resolution, thin cut, CT w/out contrast inspiratory and expiratory, and prone and supine is performed. Here are some key images Remember to apply Pulm PEEPs’ LAMBS approach to reading CTs with diffuse parenchymal findings
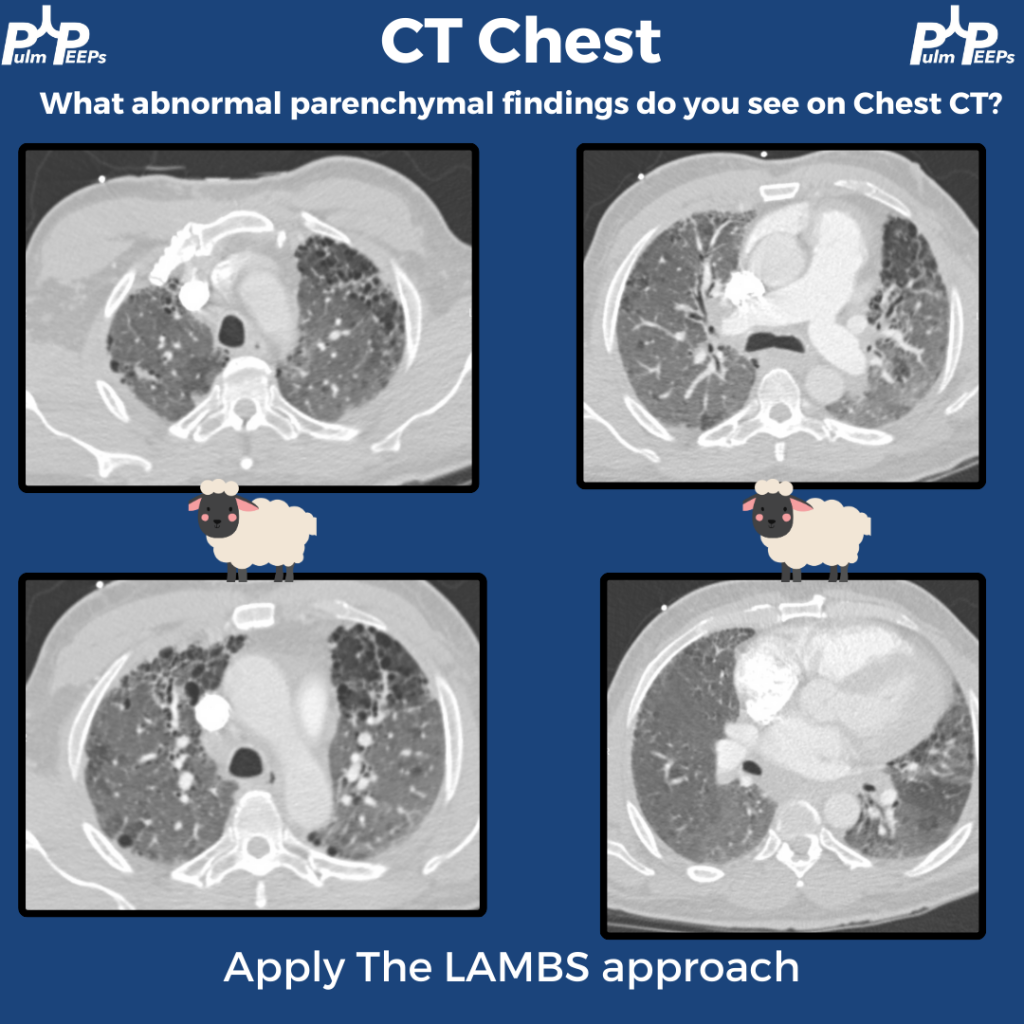
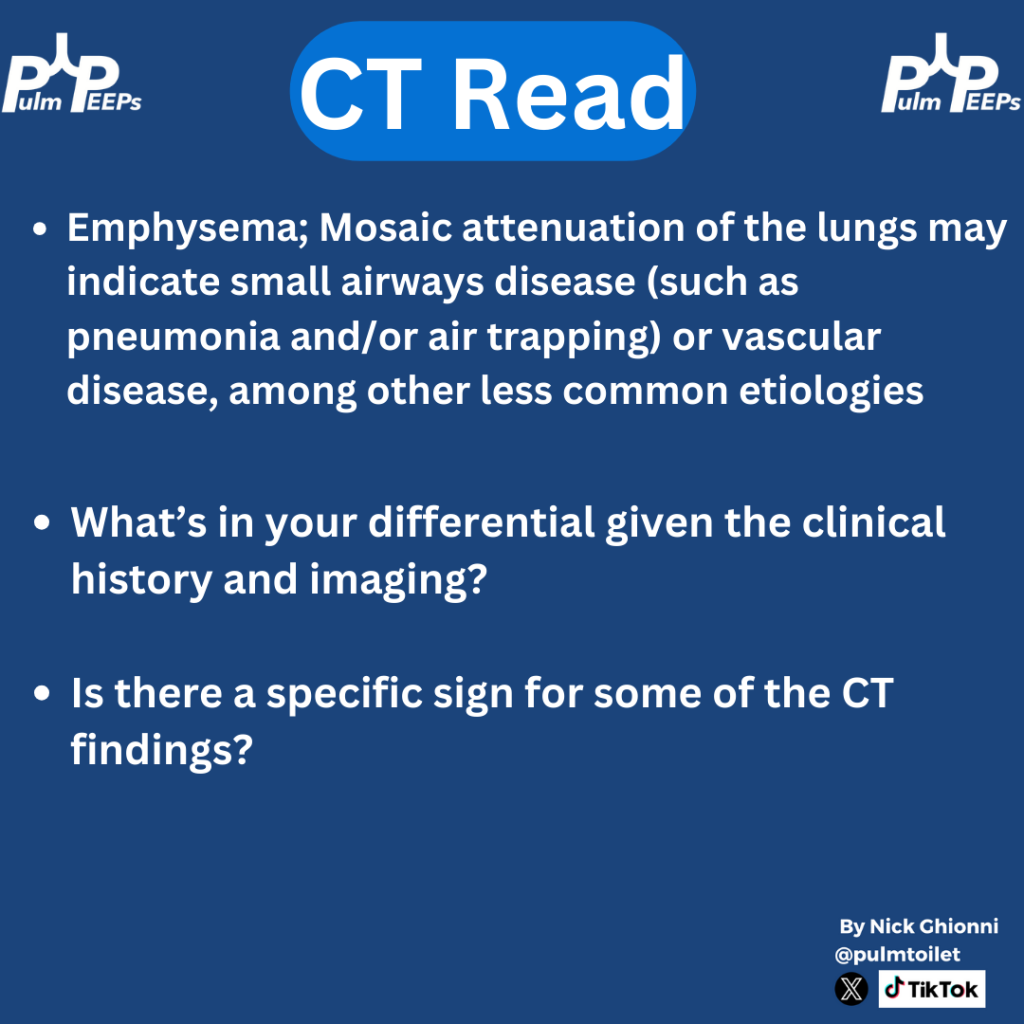
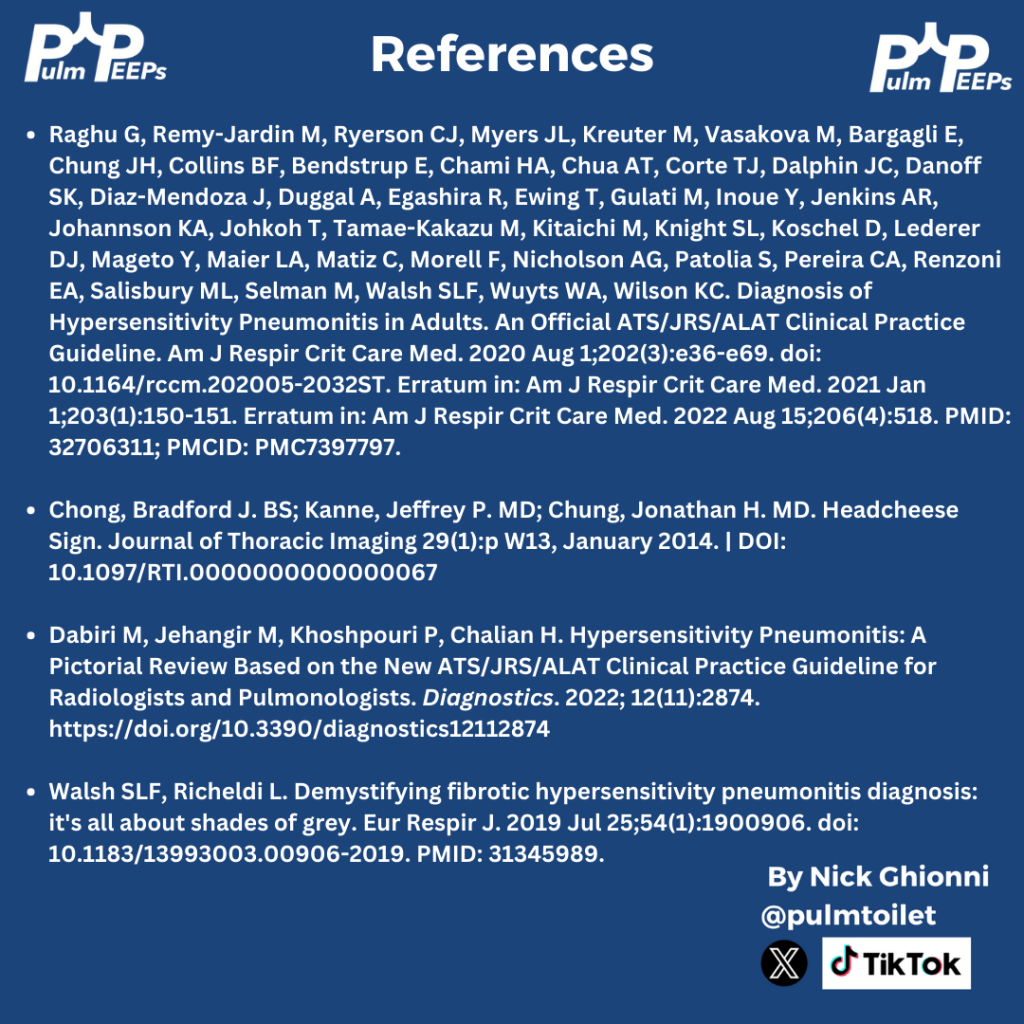
The CT scan shows an example of Triple Density Sign (formerly Headcheese Sign). This finding of areas of normal lung, high attenuation GGOs, and lucent regions of air trapping scattered throughout the lung is a specific, but not sensitive sign for fibrotic HP