Today, we’re virtually visiting the University of Virginia for another Fellows’ Case Files. This is a fantastic case that covers ARDS, the infectious work up of an immunosuppressed patient, and the evaluation of undifferentiated shock. Please let us know what you think of the episode and always feel free to reach out with interesting cases!
Meet Our Guests
John Popovich completed his residency training and chief year at UVA and has stayed on there for his pulmonary and critical care fellowship.
Tim Scialla is an associate professor of medicine at UVA. He completed his residency and fellowship at Johns Hopkins Hospital where he was also an ACS. His clinical and research focuses are advanced airways disease. He is also the program director of the PCCM fellowship.
Matt Freedman completed his residency training at Virginia Commonwealth University and is currently a second year fellow at University of Virginia.
Case Presentation
Patient: 52-year-old male with psoriasis, HIV/AIDS (CD4 count: 71), presenting with progressive shortness of breath, fever, non-productive cough, and weight loss.
Vital signs: Febrile (103°F), tachycardic (HR 110), hypoxemic on 6L O₂ (SpO₂ 90–92%).
Exam: Diffuse crackles, ill-appearing.
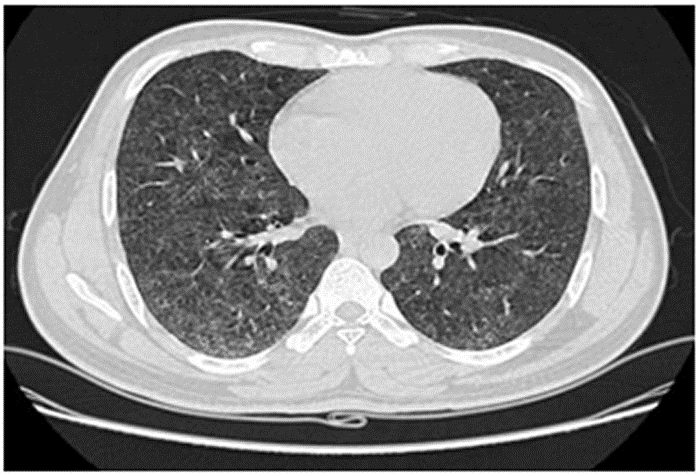
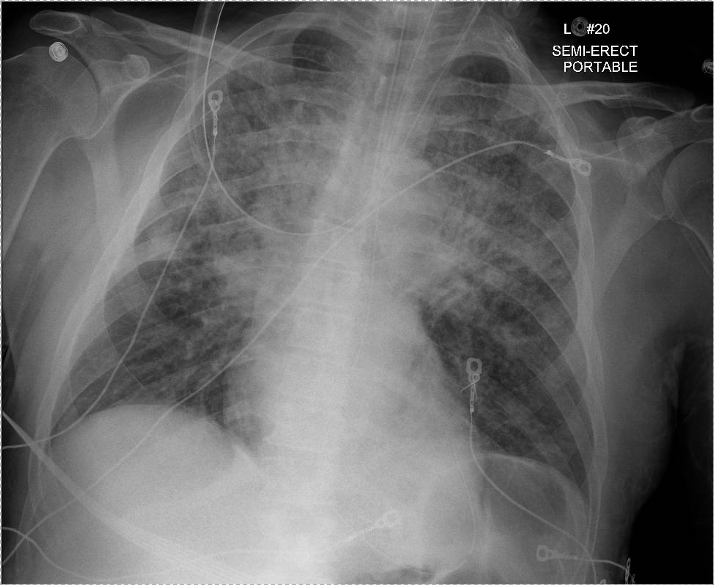
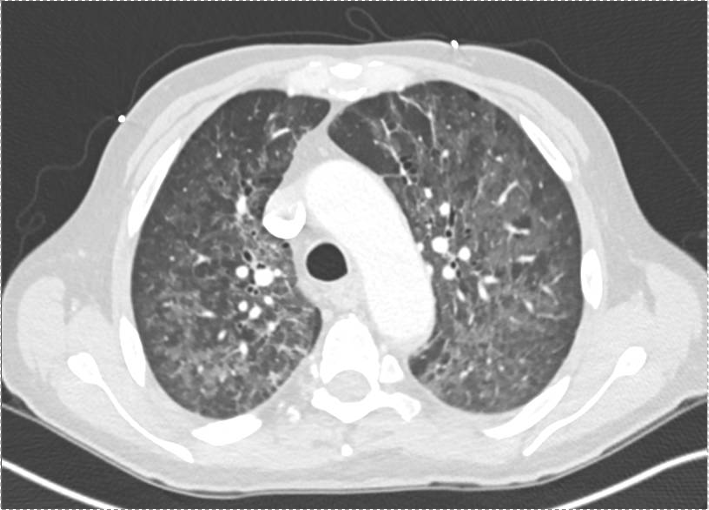
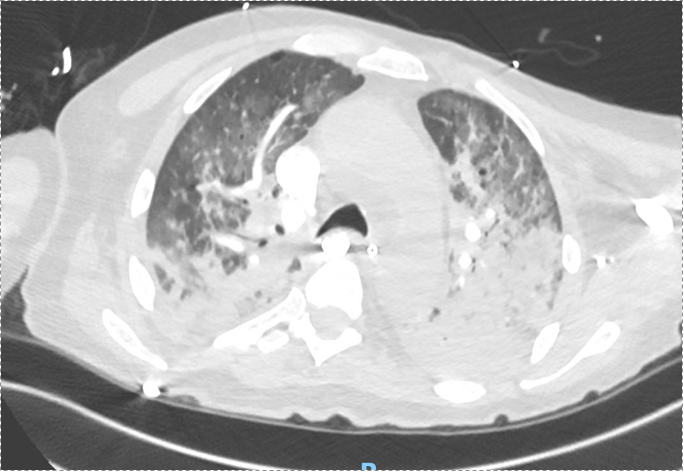
Imaging: CXR and CT showed bilateral upper lobe infiltrates, ground-glass opacities, septal thickening, and peripheral cystic changes.
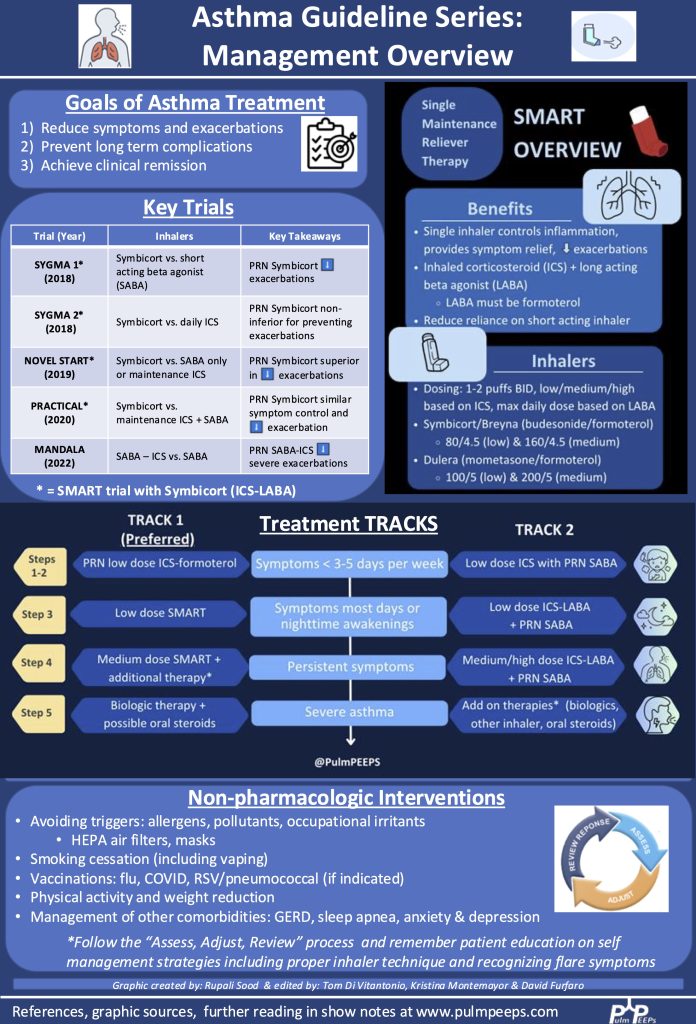
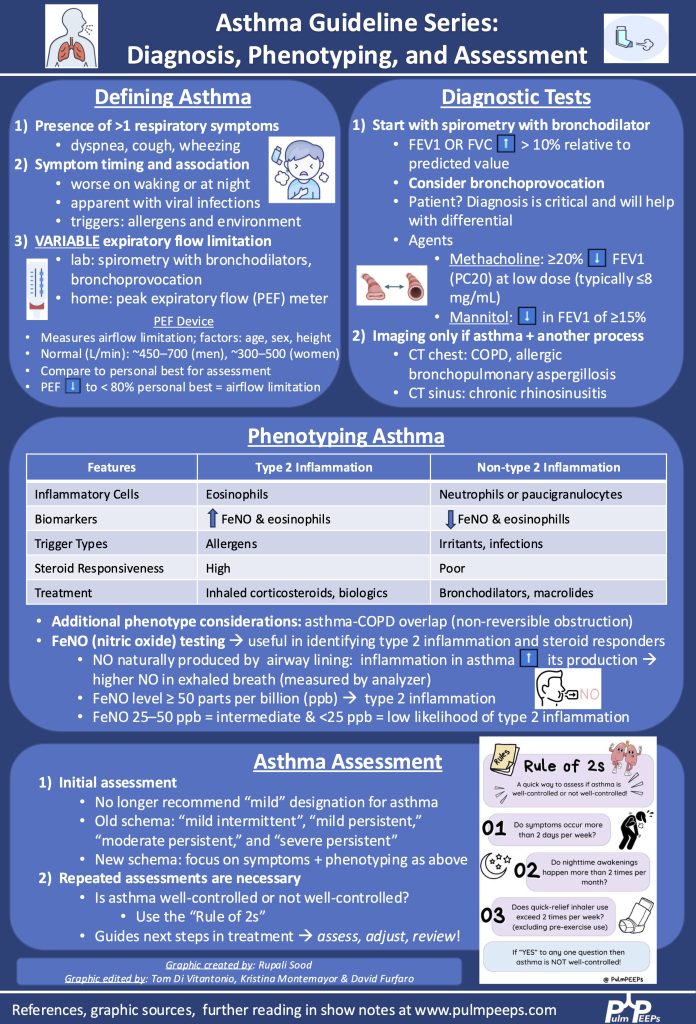
Infographics
Shock physiology:
Key Learning Points
Diagnostic Reasoning in Immunocompromised Hosts
- Framework: Anchor the differential based on type of immunosuppression.
- HIV/AIDS → T-cell dysfunction, affecting susceptibility to PCP, TB, CMV, fungi (e.g. histo/blasto), and common CAP organisms.
- PCP considerations:
- PCP can occur despite prophylaxis (e.g. Bactrim), especially if adherence or resistance issues exist.
- Classic symptoms in AIDS: acute, febrile, hypoxemic respiratory failure.
Use of Serum Markers and Imaging
- LDH: Elevated in PCP, but non-specific. High negative predictive value when normal.
- 1,3-β-D-glucan: Elevated in PCP and other fungal infections. Very sensitive for PCP (up to 95%).
- Imaging: Ground-glass opacities with cystic changes support PCP diagnosis.
Role of Bronchoscopy and Diagnostic Yield
- BAL studies to obtain:
- DFA for PCP (rapid, high specificity, lower sensitivity)
- PCR for PCP (higher sensitivity, slower turnaround)
- Cultures: bacterial, fungal, mycobacterial
- Cytology, galactomannan, histo/blasto urine antigens
- Bronch Risk-Benefit:
- Can change management in 40–60% of cases.
- Complication rate: ~10–15%, most often hypoxemia.
- Heuristic for pre-bronch ABG on non-rebreather:
- PaO₂ >150 → likely safe
- 100–150 → ~25% risk of intubation
- <100 → high risk of decompensation
Steroids in PCP and Severe CAP
- Steroids indicated in PCP with significant hypoxemia (PaO₂ <70 mmHg).
- With new CAP guidelines (Cape Cod trial), steroids may also be considered in severe bacterial CAP.
Shock Evaluation in ICU
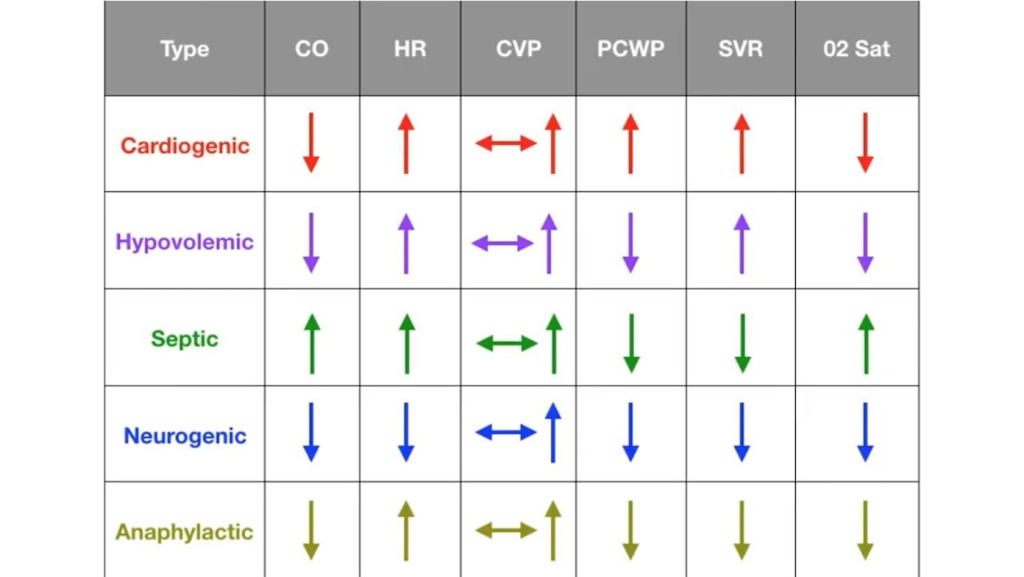
- Framework: Simplify into likely causes — distributive most common, but rule out cardiogenic, obstructive, hypovolemic.
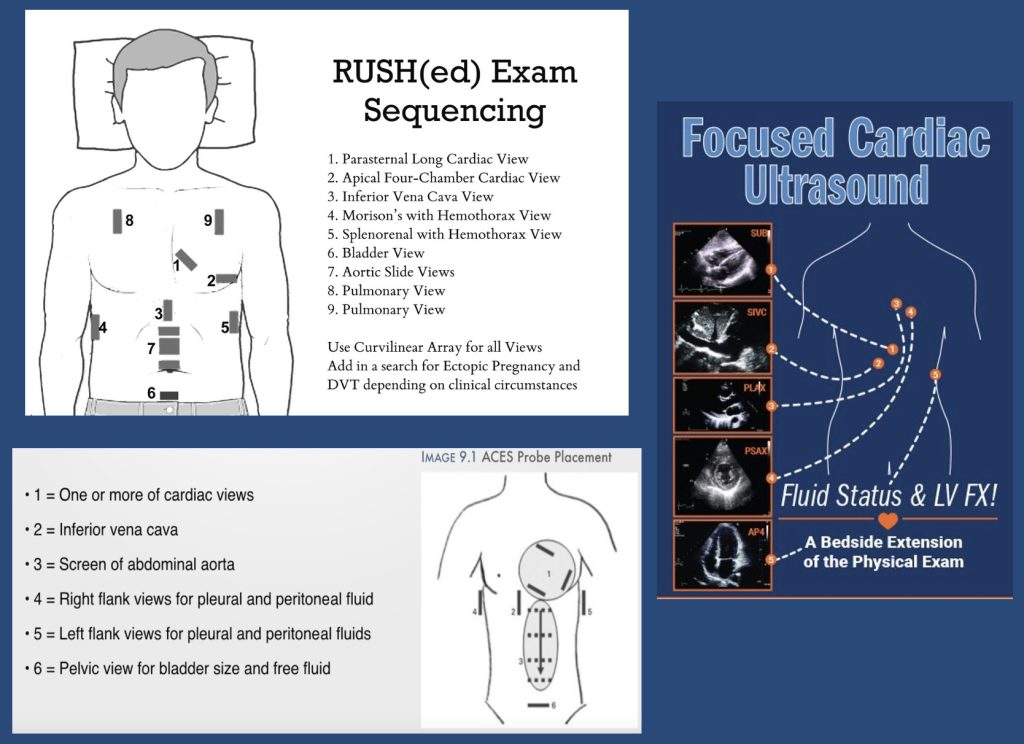
- Physical exam + POCUS essential early.
- POCUS: cardiac views, IVC, lung US, abdominal free fluid.
- Low EF doesn’t exclude distributive shock.
- PA catheter (Swan) utility:
- Useful when physiology unclear or when tracking response to therapy is critical.
- Swan data in this patient: low CVP and wedge, high SVR → distributive shock, not cardiogenic despite low EF.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More