We’re very excited this week on Pulm PEEPs to be resuming our Roundtable series. We are joined by two outstanding critical care doctors to discuss precision medicine in the ICU, specifically ARDS phenotypes. This is a topic of increasing clinical and research interest, and personalized medicine in the ICU will certainly change the landscape of how care is delivered in the coming years and decades. We are honing in on ARDS today and how phenotyping can influence future research and clinical care.
Meet Our Guests
Carolyn Calfee is a Professor of Medicine and Anesthesia at the University of California, San Francisco. She is a leader in the field of ARDS research and a pioneer in the field of ARDS phenotyping research. She has received numerous NIH grants and has literally 100s of publications on ARDS and other topics. She is also a previous ATS CC Assembly chair, and in 2022 received the ATS Recognition Award for Scientific Accomplishments.
Annette Esper is an Associate Professor of Medicine at Emory University School of Medicine. She works clinically in critical care and is the Medical Director of the stepdown Intensive Care Unit at Grady Memorial Hospital. In addition to her clinical activities, Annette does both clinical and translational research in ARDS, and was the Assembly Chair for the ATS Critical Care Assembly from 2021 – 2022.
Key Learning Points
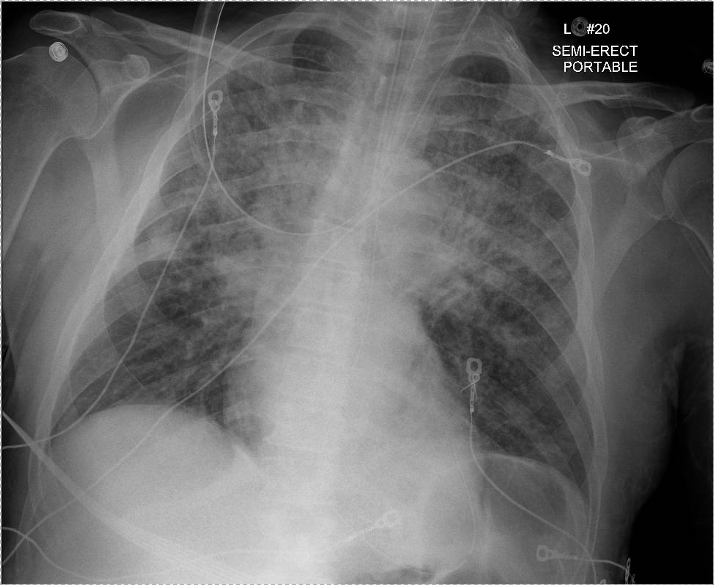
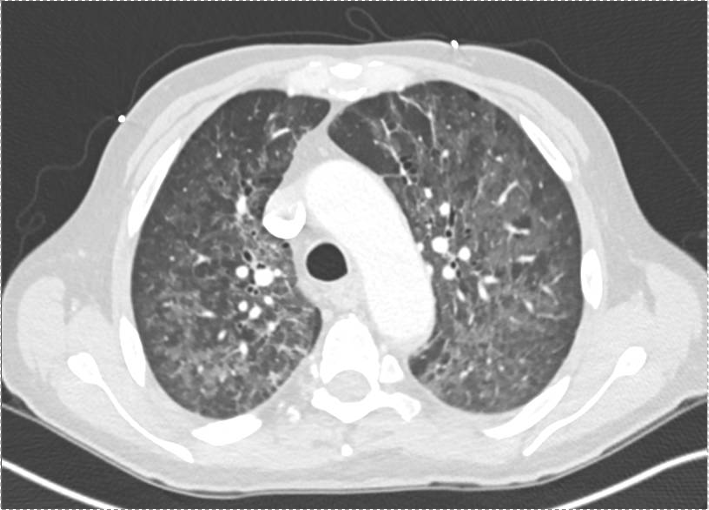
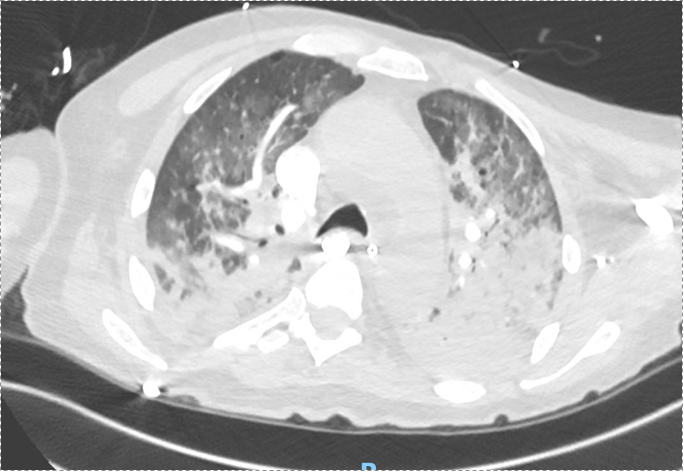
Berlin Criteria of ARDS:
— Acute symptoms developing within 7 days of a known insult
— Bilateral airspace opacites on chest imaging
— Hypoxemia not fully explained by cardiogenic pulmonary edema
— P:F ratio < 300 on a PEEP of 5
Heterogeneity in ARDS
— ARDS has a broad definition so it is comprised of people with a wide range of disease characteristics and severity
— There is heterogeneity in clinical characteristics, but also underlying biological drivers of disease
— Heterogeneity stymies research efforts to identify effective therapies in ARDS
Phenotyping in ARDS
— There are many ways of phenotyping for critical illness and ARDS
1. Etiology. Examples: COVID vs non-COVID, pulmonary vs non-pulmonary, bacterial vs viral
2. Physiologic phenotypes: Severity (Berlin criteria P:F ratio); Compliance, Ventilatory ratio
3. Biological phenotypes: Different underlying drivers of disease
— The motivation for phenotyping is to find treatment-responsive subgroups within the broader heterogeneous subgroups
— Phenotyping embodies more than risk factors, because it includes information about the host response, not just predictors of outcome
Biomarkers in ARDS
— There is probably a role for biomarkers in ARDS clinically and in research
> Prognostication
> Identify who will be responsive to specific therapies
> May not be one biomarker, will likely be a panel
— What is the perfect ARDS biomarker?
> Specific: identify a group of patients that are at risk, or respond to therapies differently
> Easily measurable at the bedside
> Reliable
> Reproducible
— Challengers in identifying useful biomarkers
> Heterogeneity of disease
> Real world applicability. For example, can you get IL-6 back in real-time? Can you apply it consistently when labs have different testing techniques and scales?
> Temporal stability – how do biomarkers change over the time course of ARDS?
— Biomarkers of interest
> Inflammatory markers (IL-6, IL-8, TNF)
> sRAGE – Soluble receptor for advanced glycation end products
> Highest levels on type 1 alveolar epithelial cells
> Seems to be a marker of alveolar epithelial injuries
> Meta-genomic sequencing of patients in a real-time environment
Latent class analysis
— Clustering technique that, agnostic to outcomes, looks for existing groups within the data
— Ideally, identifies biologically distinct phenotypes that may have different prognoses or response to therapy
Omics in ARDS
— Existing risk scores are quite limited, so using biological data to distinguish patients seems promising.
— Unbiased approach to identifying subgroups to identify patients that behave similarly biologically
— Omics is really thinking about endotyping patients and identifying the biological processes that are driving phenotypes
Hypo and hyperinflammatory phenotypes in ARDS
— Described by LCA incorporating demographics, clinical data, labs, vital signs, 6-8 plasma protein biomarkers
— Importantly, the groups were identified agnostically to outcomes.
— Distinguished by:
> Inflammatory biomarkers (IL-6, IL-8, TNF 1)
> Acidosis
> Shock, vasopressor requirement, and multi-system organ failure
— Consistently across 8 different data sets
— Both RCTs and observational cohorts
— Hyperinflammatory phenotype has dramatically worse clinically outcomes (higher mortality, fewer VFD)
— The different phenotypes respond differently to therapies retrospectively in RCTs
— The phenotypes did respond differently to PEEP, fluids conservative therapy, and simvastatin.
— This was not seen universally (rosuvastatin did not have differential treatment response)
— Note: We don’t really know that inflammation is at the heart of the pathogenesis of what distinguishes these two groups. The “hypoinflammatory” phenotype still has elevated levels of inflammatory biomarkers compared to controls.
What is next?
— This is all just subgroup analysis.
— These hypotheses still need to be tested prospectively
— Need to be able to easily identify the phenotypes quickly and easily
— Working on biomarker-based and non-biomarker-based clinical classifications
Key Quote:
Dr. Calfee “My takeaway point would be, there is no one best or one right way to phenotype these patients. I think there are numerous different approaches that we’re probably going to be using over the years. But I would say that what we want to focus on is what has the potential to change outcomes for our patients and to really identify individual patients or groups of patients that respond differently to therapies. And I think if we can keep that goal in mind and start testing some of these hypotheses prospectively we’re going to make progress.”
References and links for further reading
- Sinha P, Calfee CS. Phenotypes in ARDS: Moving Towards Precision Medicine. Curr Opin Crit Care. 2019;25(1):12-20. doi:10.1097/MCC.0000000000000571
- Calfee CS, Delucchi KL, Sinha P, et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018;6(9):691-698. doi:10.1016/S2213-2600(18)30177-2
- Matthay MA, Arabi YM, Siegel ER, et al. Phenotypes and personalized medicine in the acute respiratory distress syndrome. Intensive Care Med. 2020;46(12):2136-2152. doi:10.1007/s00134-020-06296-9
- Wilson JG, Calfee CS. ARDS Subphenotypes: Understanding a Heterogeneous Syndrome. Crit Care. 2020;24(1):102. doi:10.1186/s13054-020-2778-x
- Yang P, Esper AM, Martin GS. The Future of ARDS Biomarkers: Where Are the Gaps in Implementation of Precision Medicine? In: Vincent JL, ed. Annual Update in Intensive Care and Emergency Medicine 2020. Annual Update in Intensive Care and Emergency Medicine. Springer International Publishing; 2020:91-100. doi:10.1007/978-3-030-37323-8_7
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | | More