We’re back with another Case Files episode from Mt. Sinai Morningside. Listen in to hear another great case and some key learning points along the way.
Meet Our Guests
Dr. Sara Luby is a third-year Internal Medicine resident and rising chief resident at Mt. Sinai Morningside/West and planning on applying to Pulmonary and Critical Care fellowship this upcoming year.
Dr. Javier Zulueta is the Chief of the Division of Pulmonary, Critical Care, and Sleep Medicine at Mount Sinai Morningside. He completed residency training at St. Luke’s Medical Center/Case Western in Cleveland and fellowship in Pulmonary/Critical Care at Tufts Medical Center in Boston. His research focuses on lung cancer screening and incidental lung findings.
Dr. Mirna Mohanraj is the Associate Program Director for the Pulmonary and Critical Care Fellowship at Mt. Sinai Morningside / Beth Israel and an associate professor of medicine and medical education at the Icahn School of Medicine at Mount Sinai. She completed residency training at University of Chicago and fellowship training at Mt. Sinai Hospital.
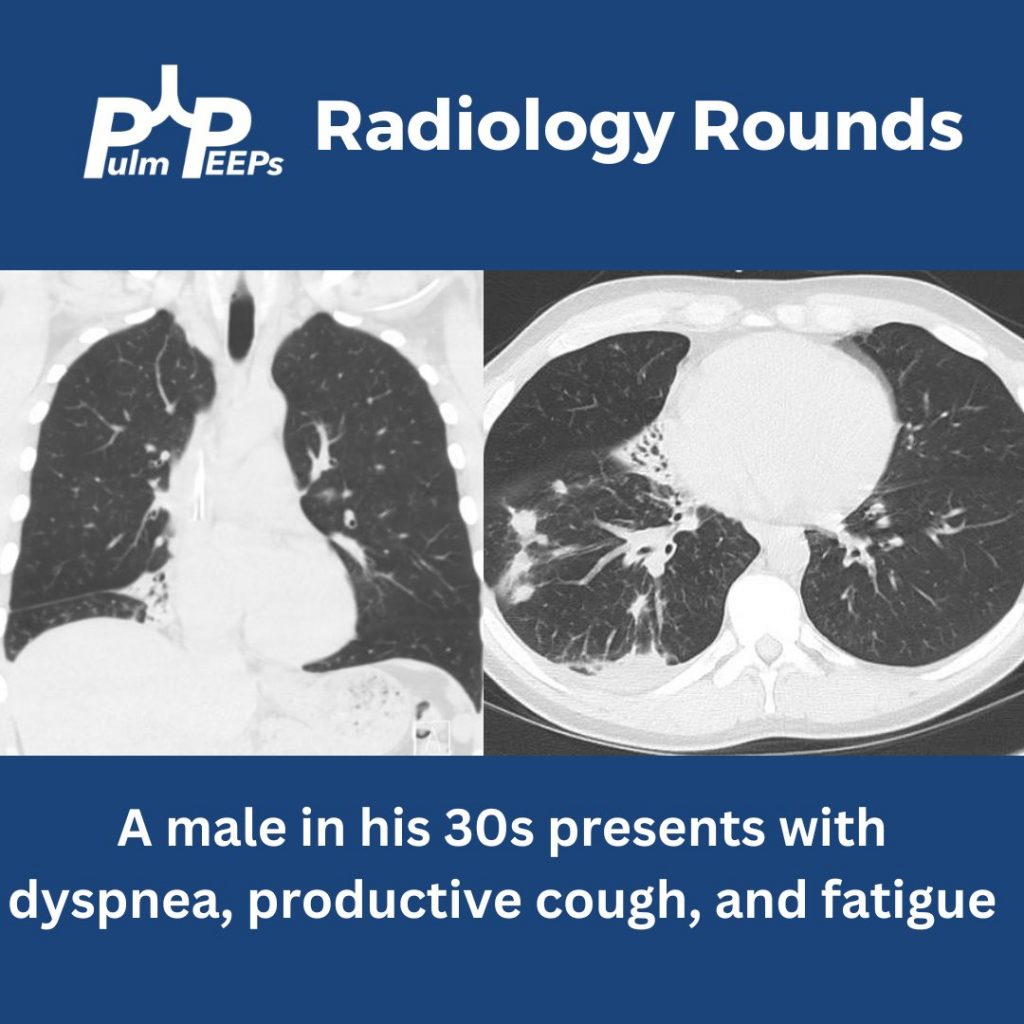
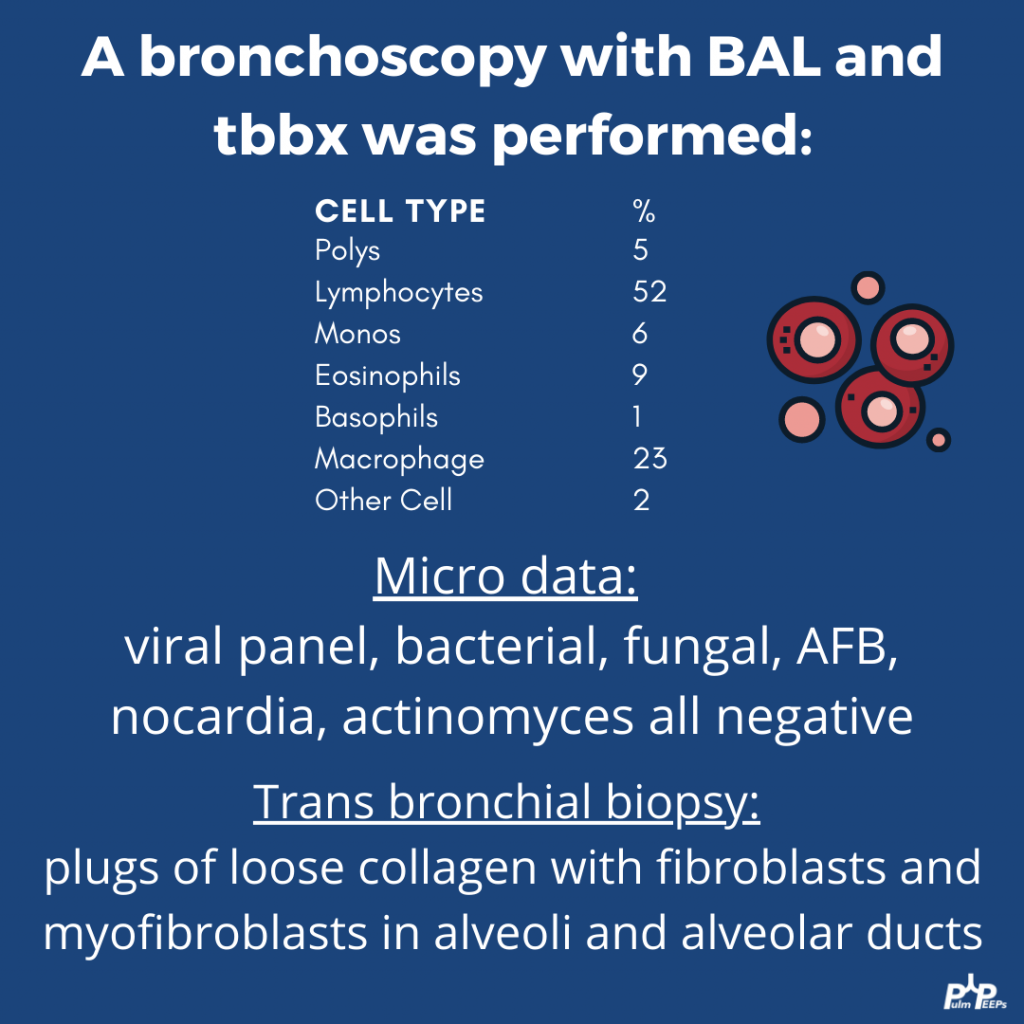
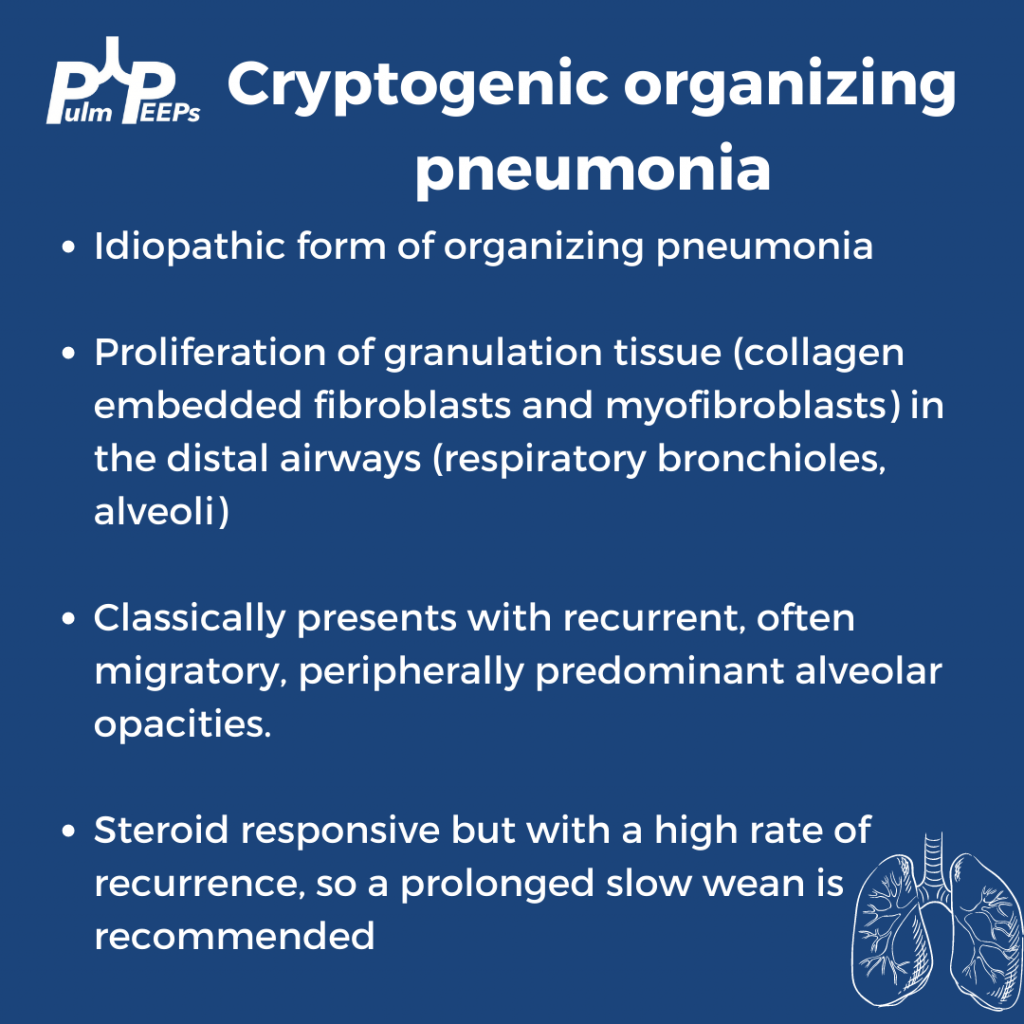
Case Presentation
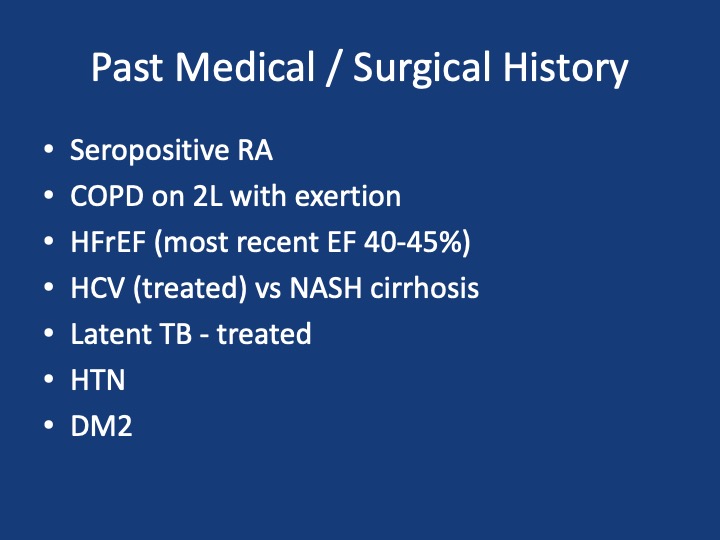
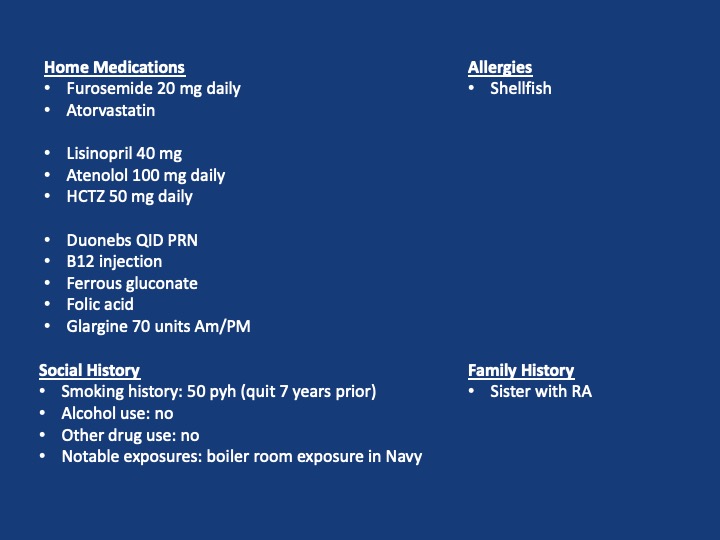
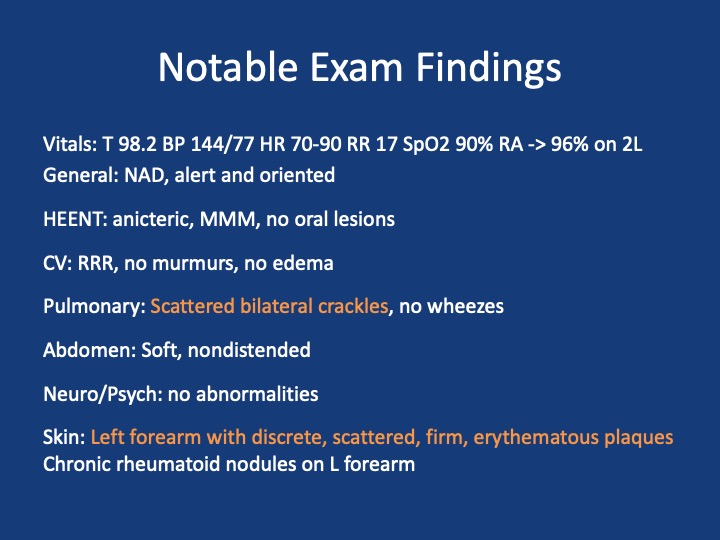
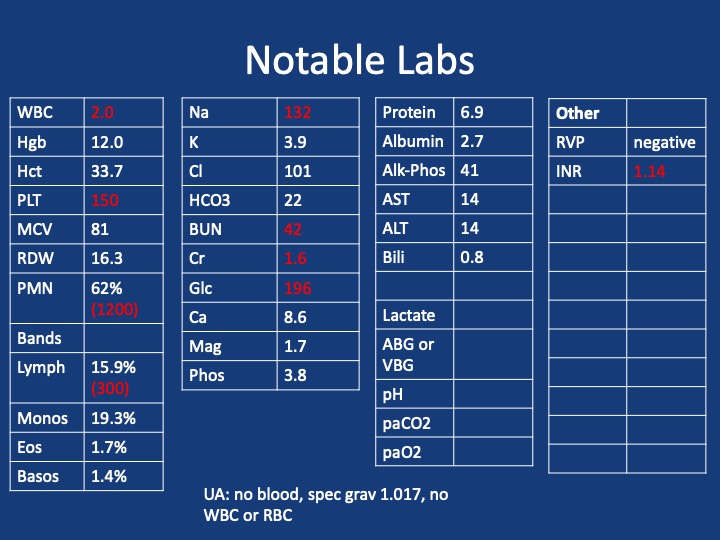
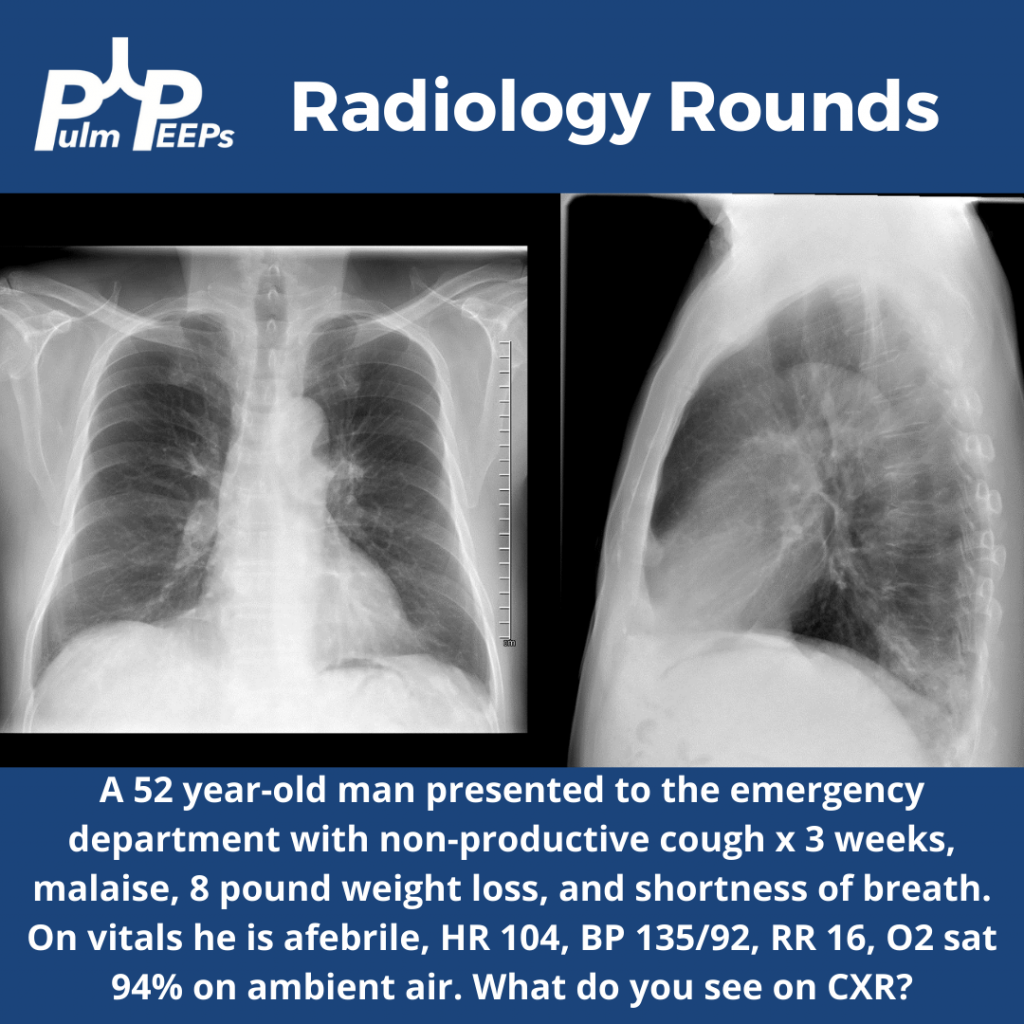
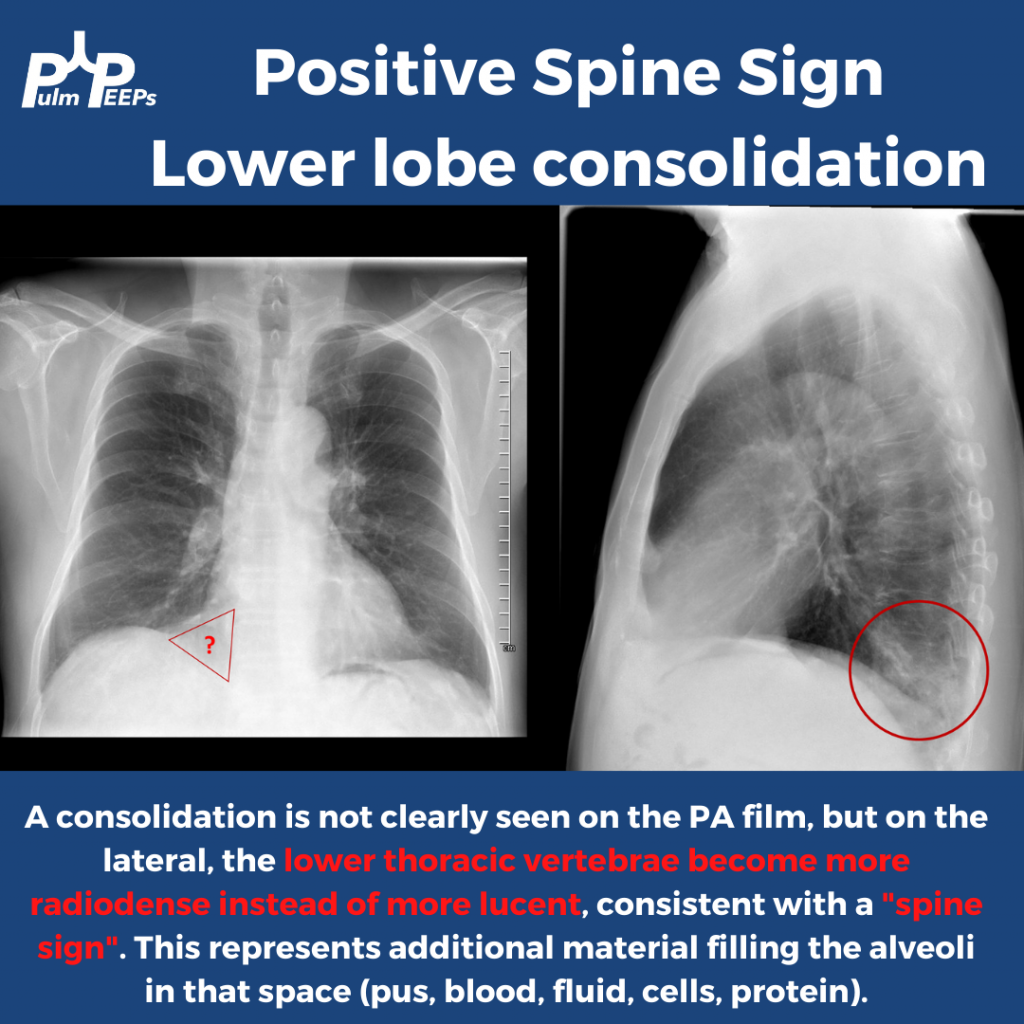
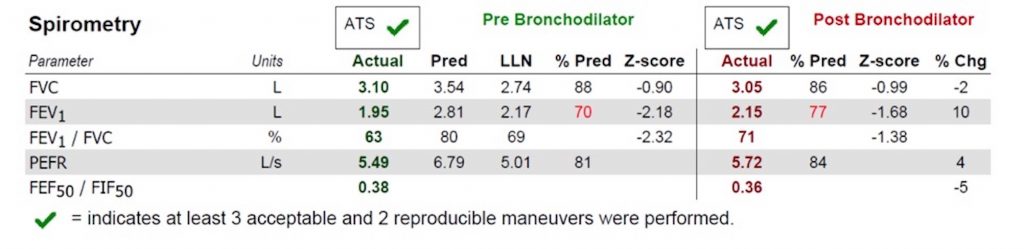
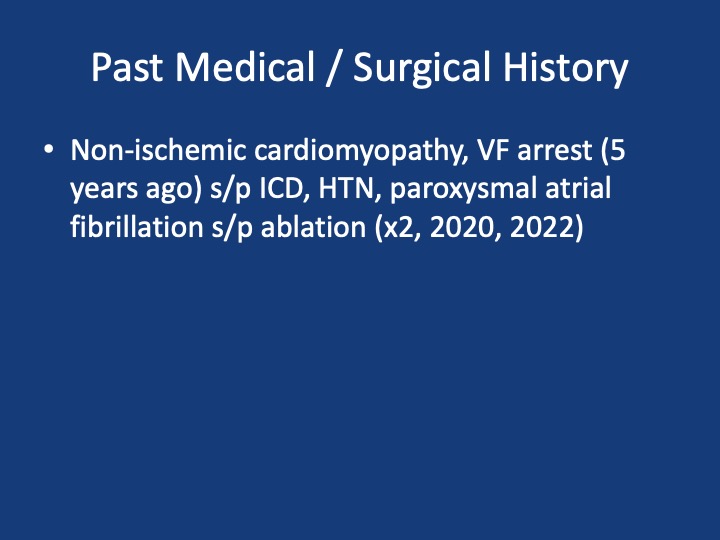
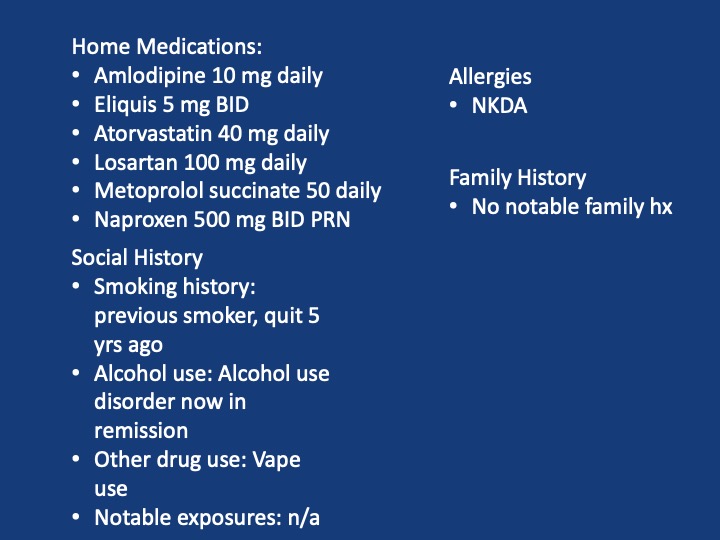
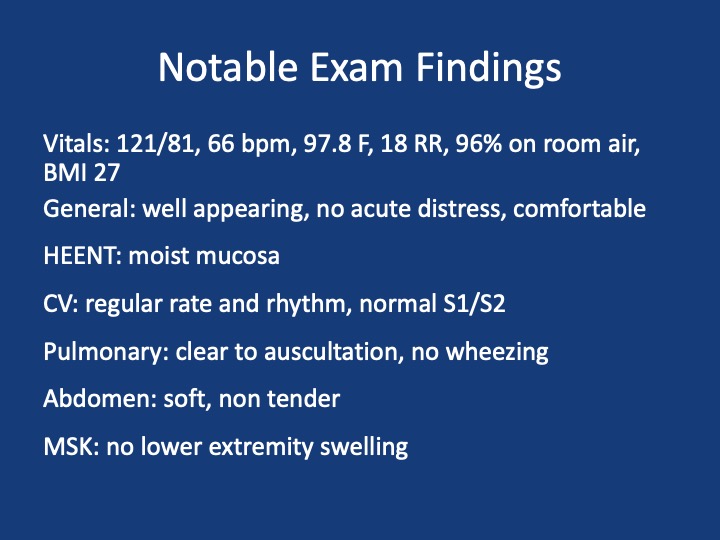
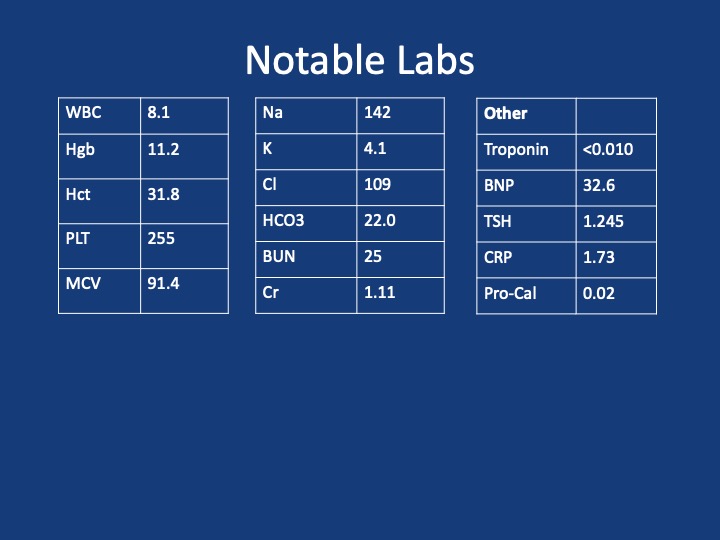
A 51 year old male presents with two days of acute on chronic chest pain and shortness of breath, worsening over the last month. His initial vitals: 143/ 100, pulse 85, temperature 36.5 °C (97.87°F), RR 16, SpO2 97 % on room air, BMI 29.8
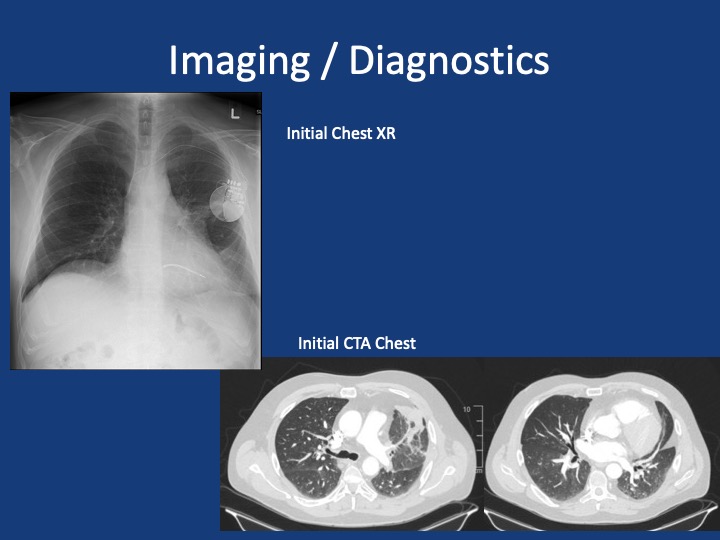
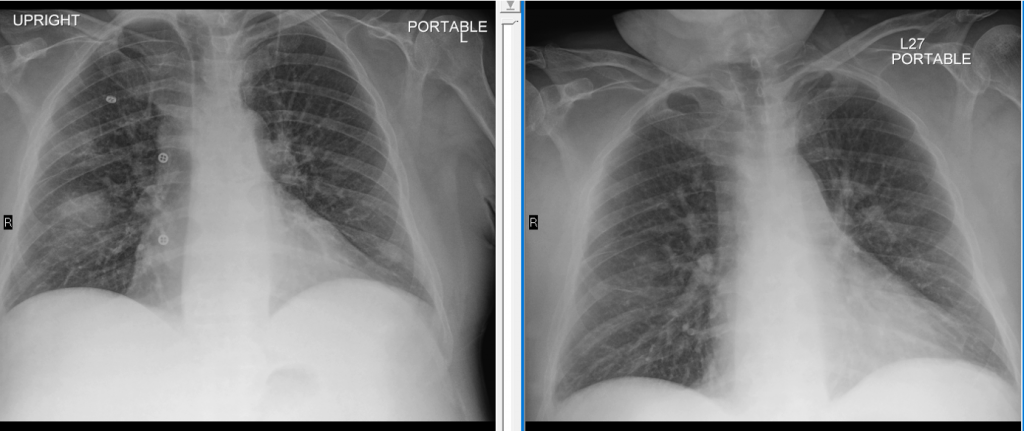
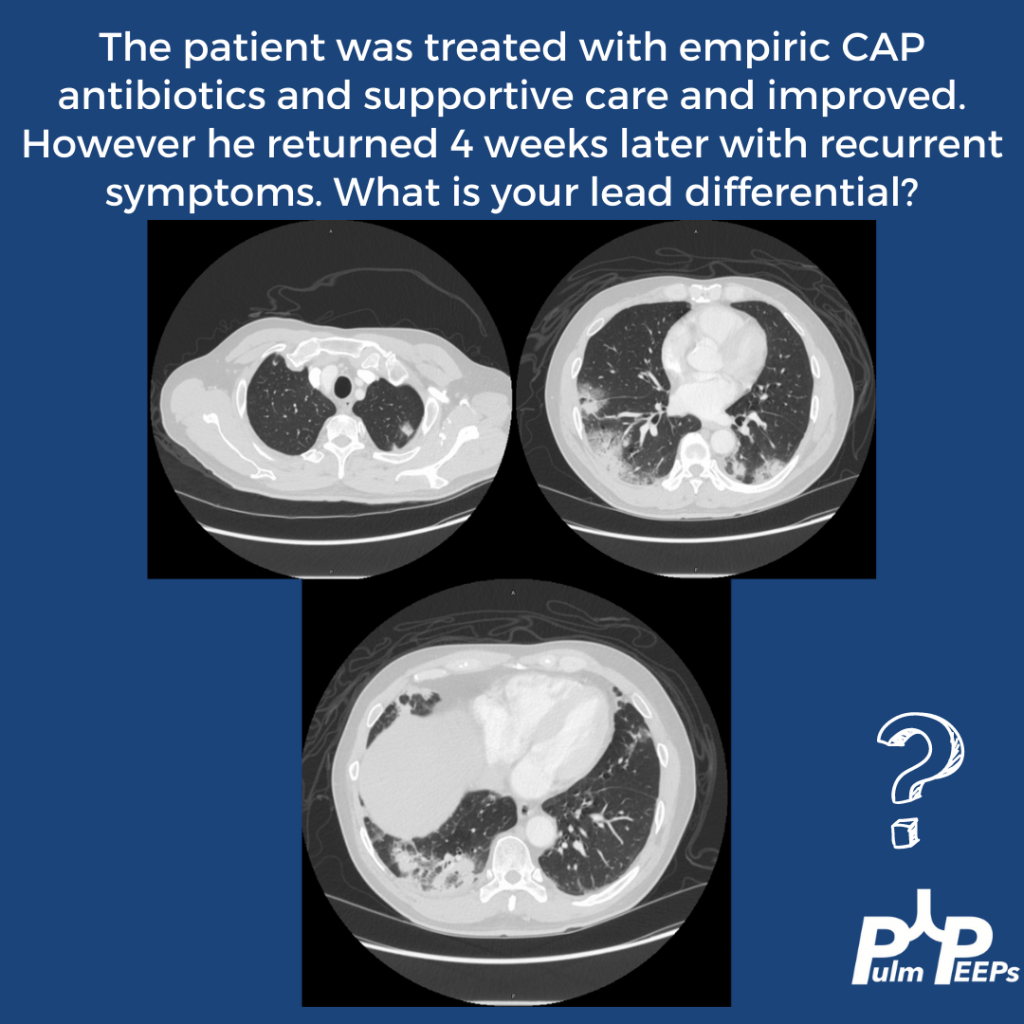
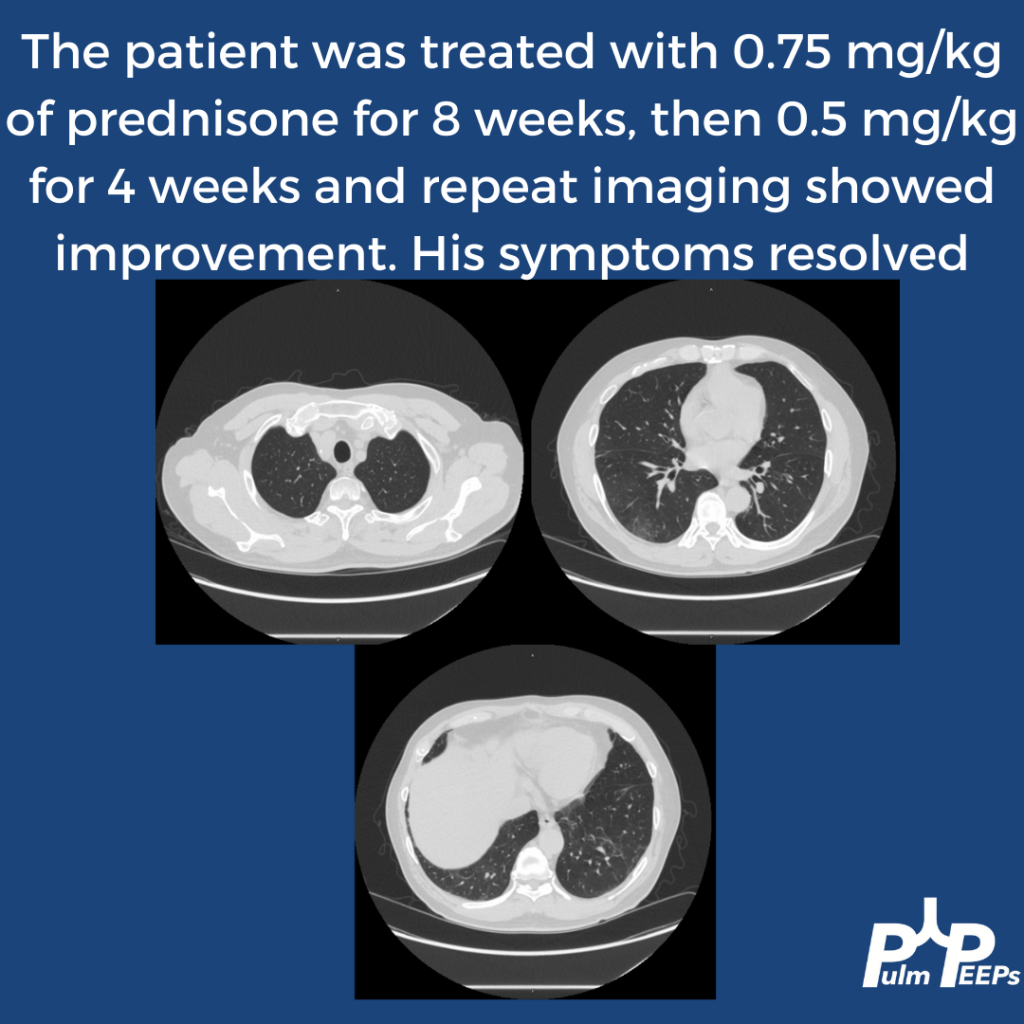
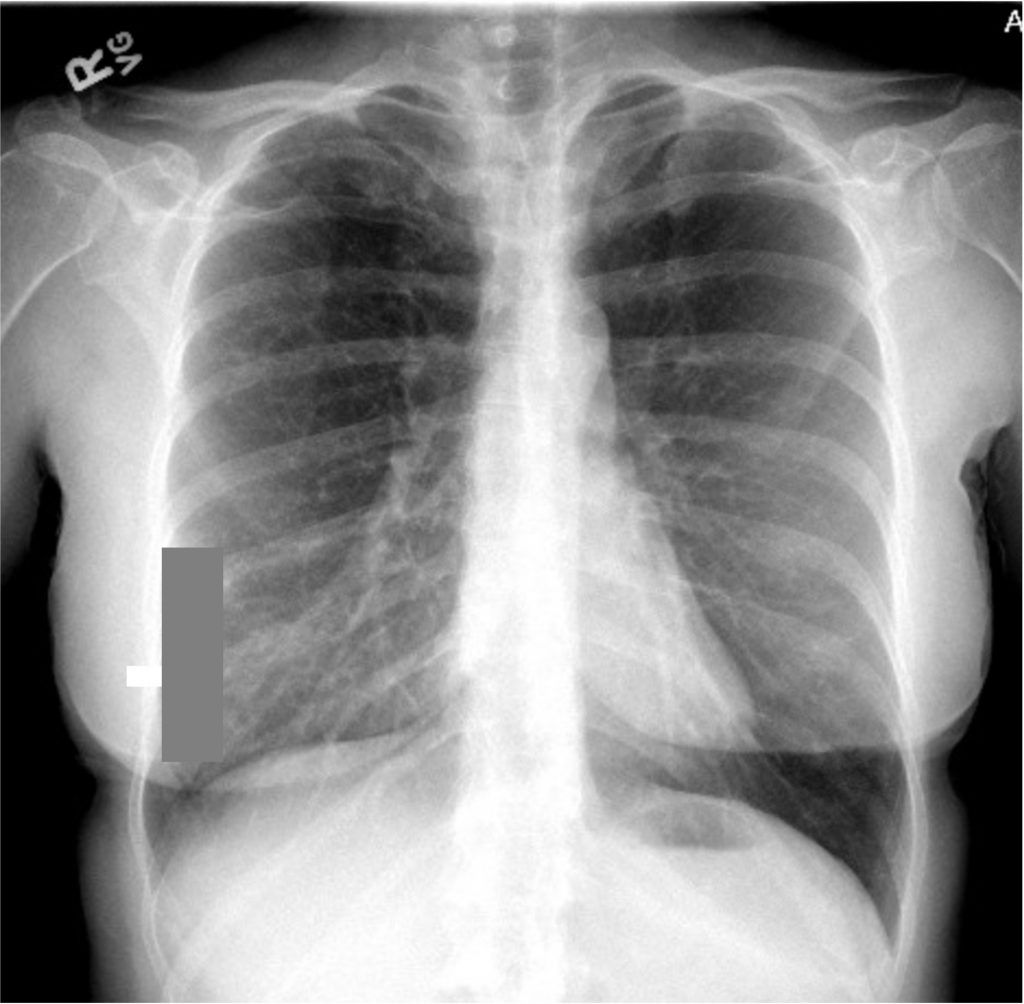
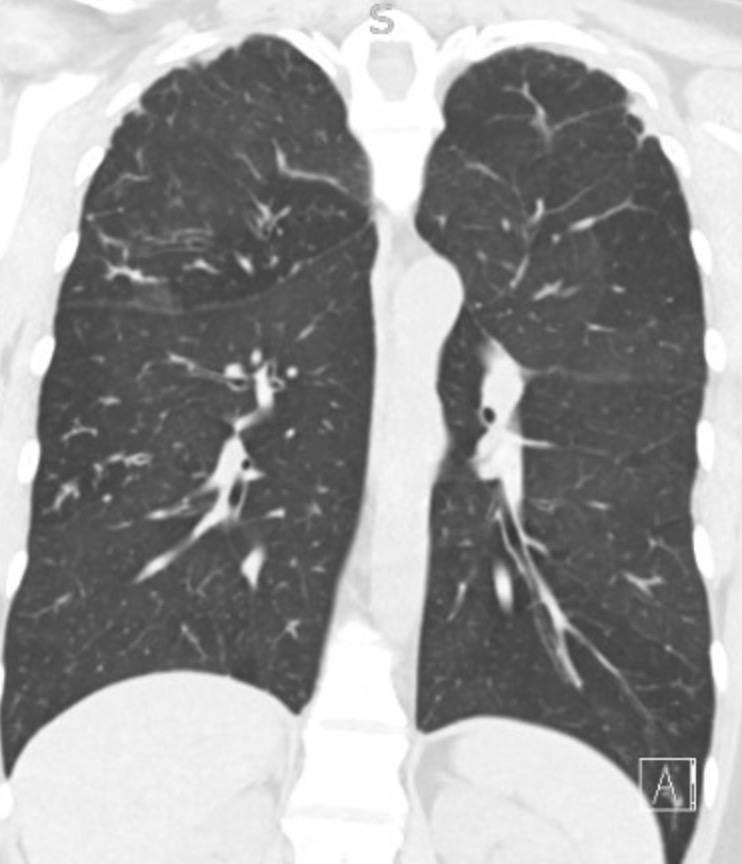
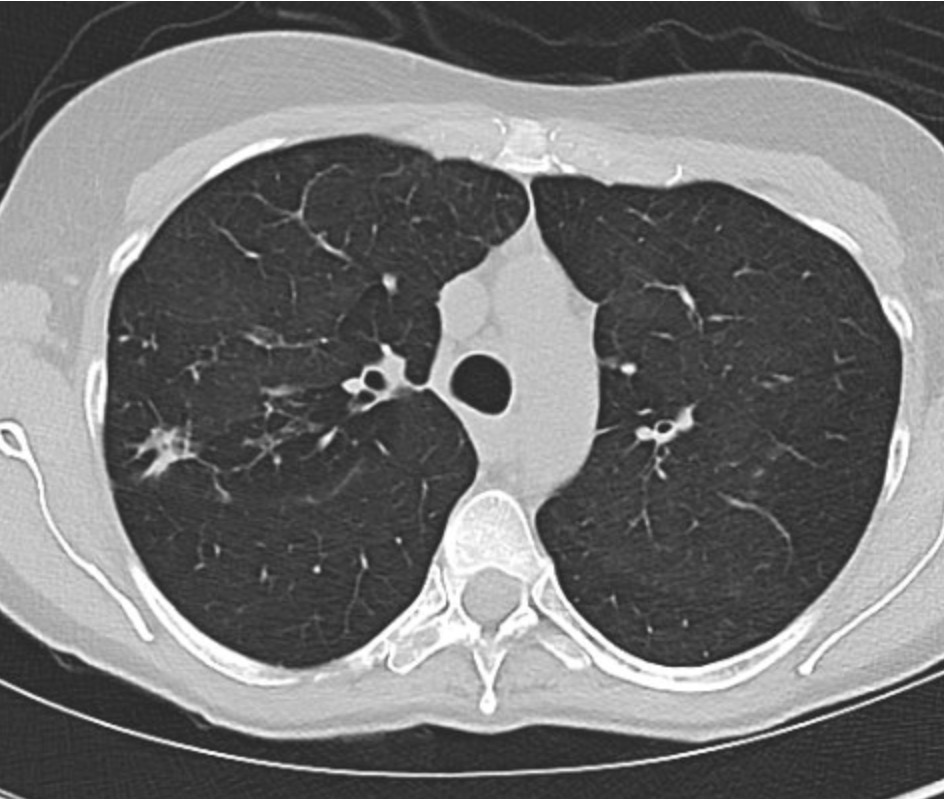
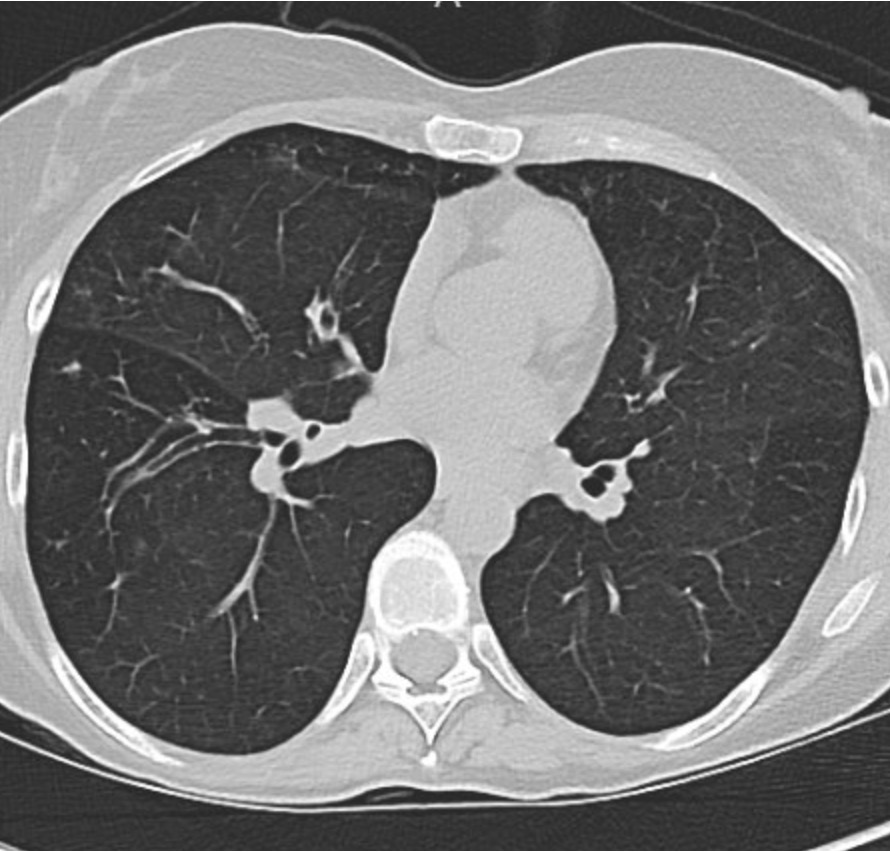
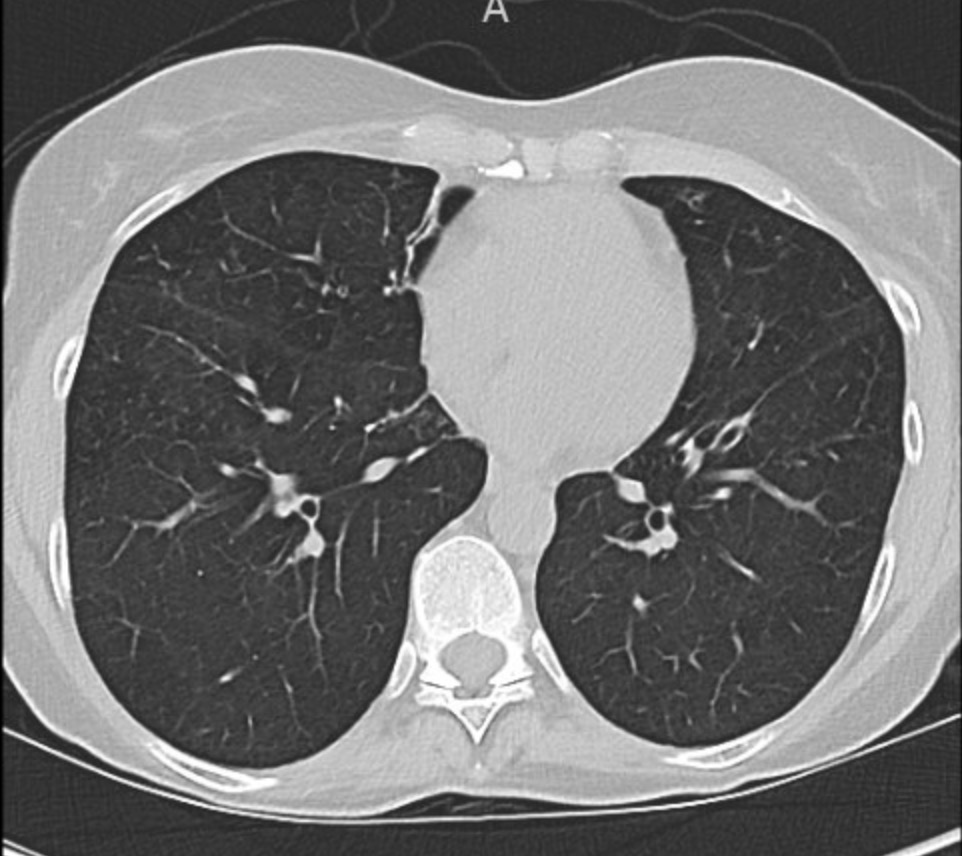
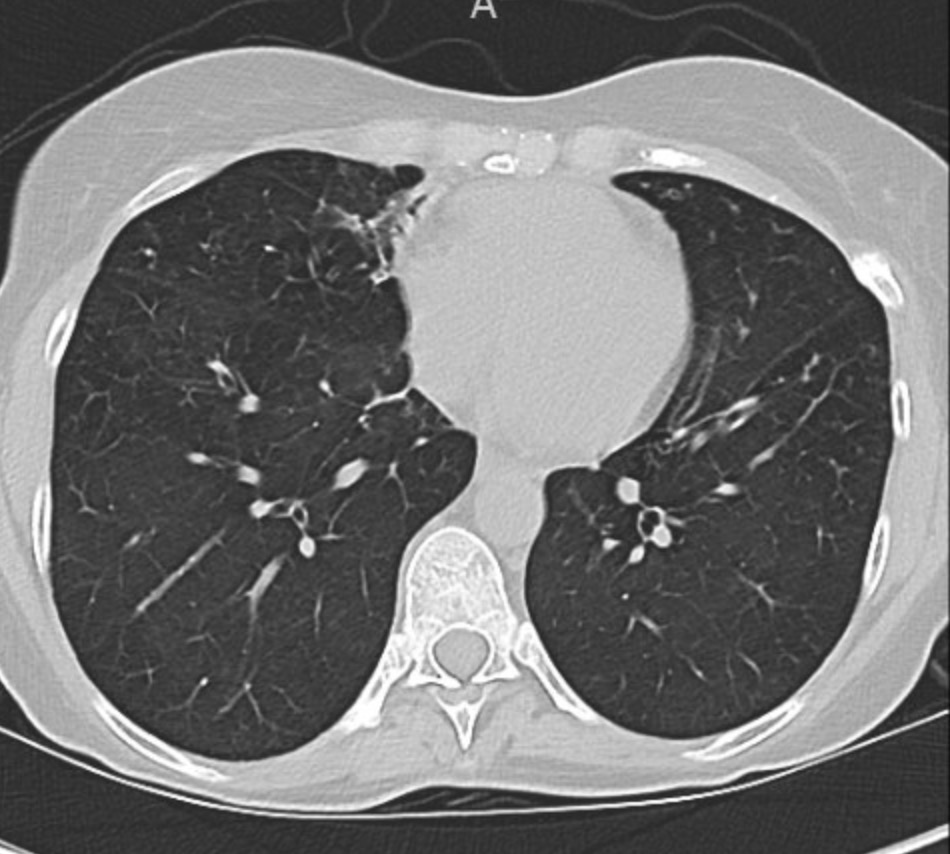
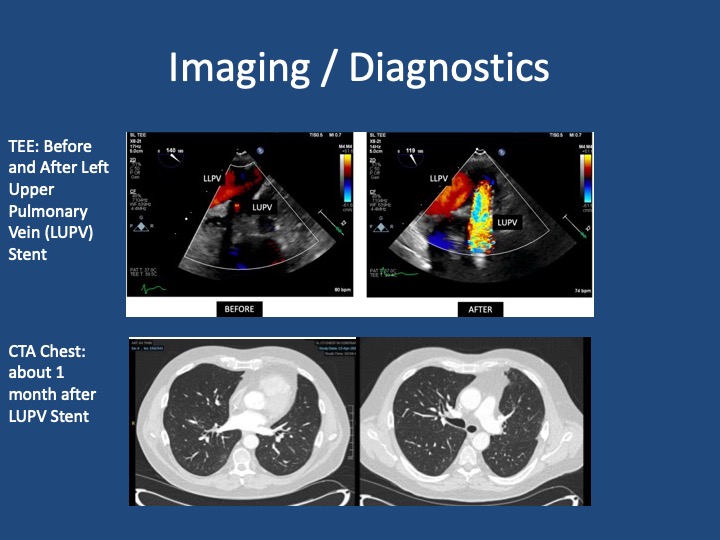
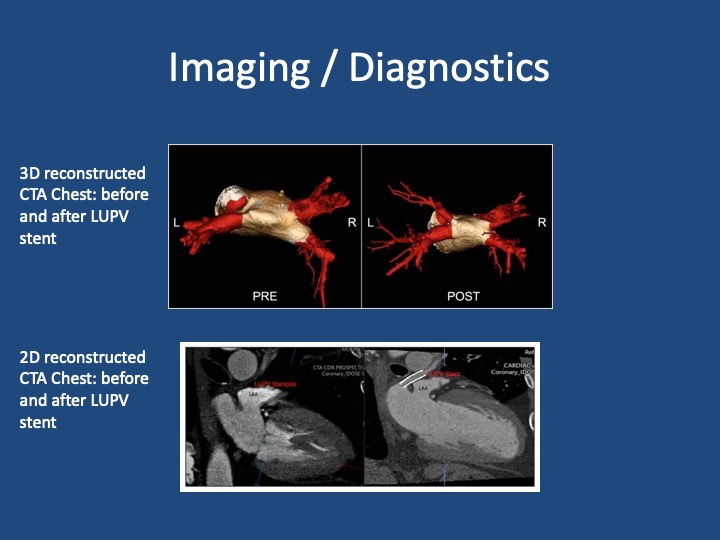
Pre and Post Treatment Imaging
References and Further Reading
Shroff N, Choi W, Villanueva-Meyer J, Palacio DM, Bhargava P. Pulmonary vein occlusion: A delayed complication following radiofrequency ablation for atrial fibrillation. Radiol Case Rep. 2021;16(12):3666-3671. doi:10.1016/j.radcr.2021.09.015
Fender EA, Widmer RJ, Hodge DO, et al. Assessment and Management of Pulmonary Vein Occlusion After Atrial Fibrillation Ablation. JACC: Cardiovascular Interventions. Vol 11(16); 2018. doi:10.1016/j.jcin.2018.05.020
López-Reyes R, García-Ortega A, Torrents A, et al. Pulmonary venous thrombosis secondary to radiofrequency ablation of the pulmonary veins. Respir Med Case Rep. 2018;23:46-48. doi:10.1016/j.rmcr.2017.11.008
Mizuno A, Mauler-Wittwer S, Muller H, Noble S. Recurrent pneumonia post atrial fibrillation ablation: do not forget to look for pulmonary vein stenosis. BMJ Case Rep. 2022;15(12):e250896. doi:10.1136/bcr-2022-250896
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More