We’re back with another edition of Fellows’ Case Files! Today, we’re virtually visiting Rutgers University, Robert Wood Johnson Medical School to work through a fascinating pulmonary case. Enjoy, and let us know your thoughts.
Meet Our Guests
Khalil El Gharib completed his residency training at Northwell at Staten Island University Hospital Program and is currently a first year fellow at Rutgers Robert Wood Johnson Medical School.
Sabiha Hussain completed her residency training at Robert Wood Johnson Medical School and her fellowship training at Columbia Presbyterian Medical Center in New York. She is currently a Professor of Medicine and the fellowship Program Director.
Case Presentation
- Patient: 28-year-old male with Asperger’s syndrome and IgA nephropathy.
- Symptoms: 3-month history of progressive dry cough and dyspnea on exertion; later developed mild hemoptysis.
- Notable exposure: Questionable black mold in the patient’s apartment.
Initial Workup and Diagnostic Reasoning
- Vital signs: Hypoxemia (SpO₂ 91% on room air).
- Exam: Inspiratory crackles.
- ABG findings: Elevated A–a gradient (~50), indicating a gas exchange problem.
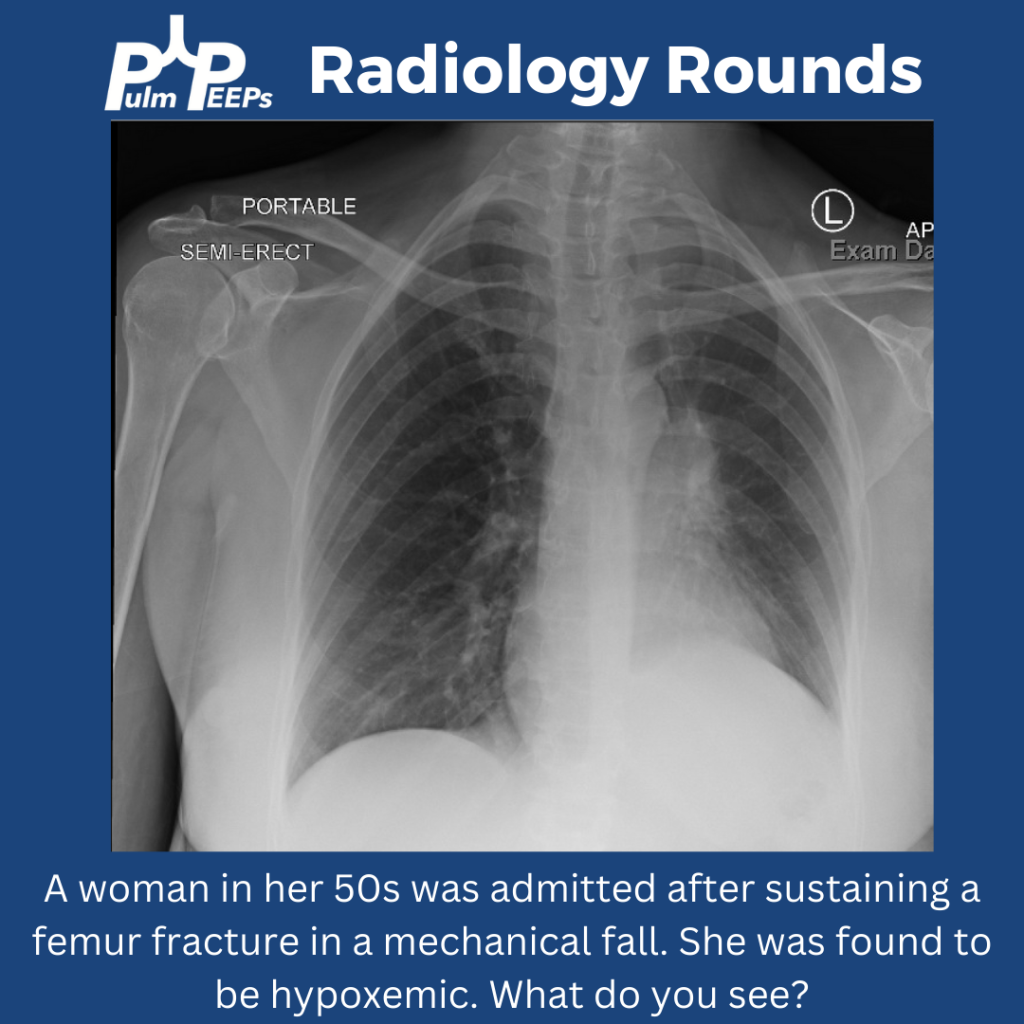
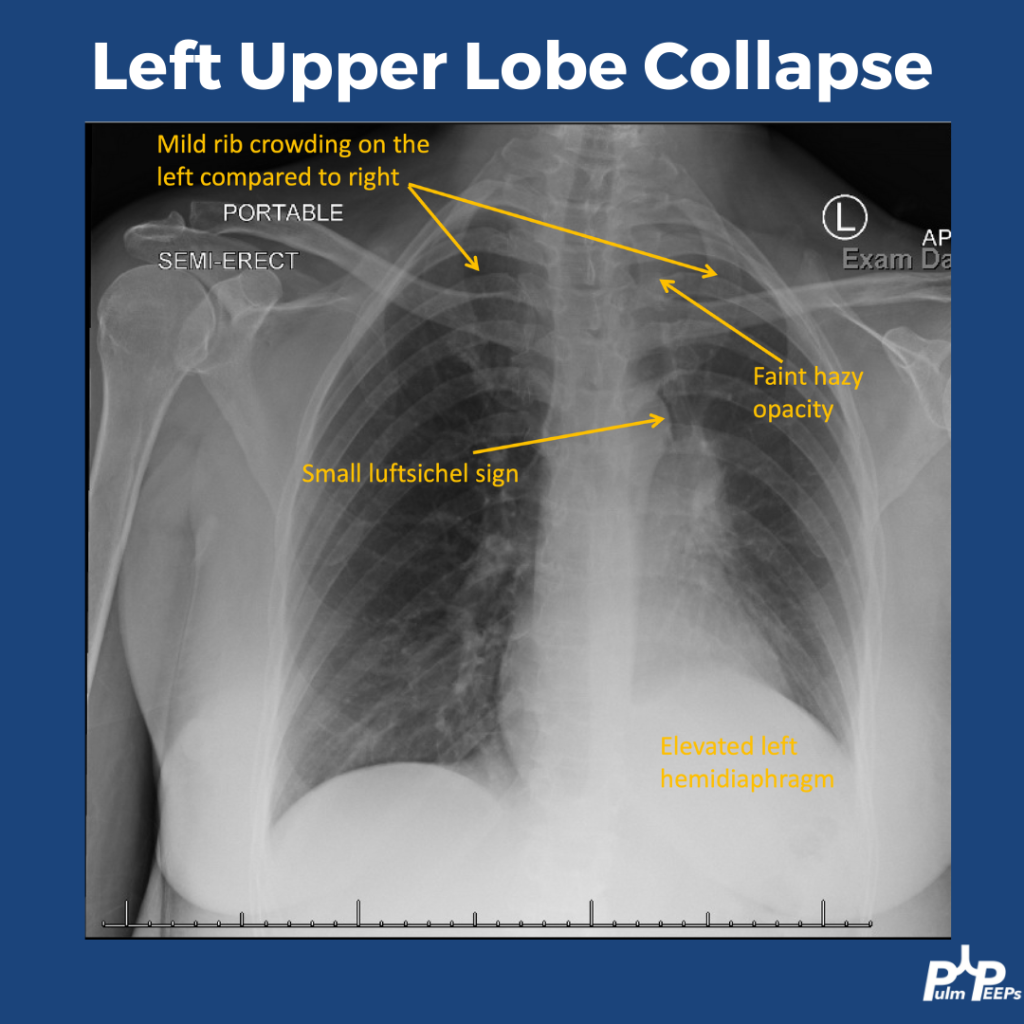
- Chest X-ray: Bilateral, patchy infiltrates without specific lobar preference.
- Initial management: Discharged with empiric antibiotics for presumed multifocal pneumonia.
Re-Presentation and Further Testing
- Symptoms worsened; now with blood-tinged sputum.
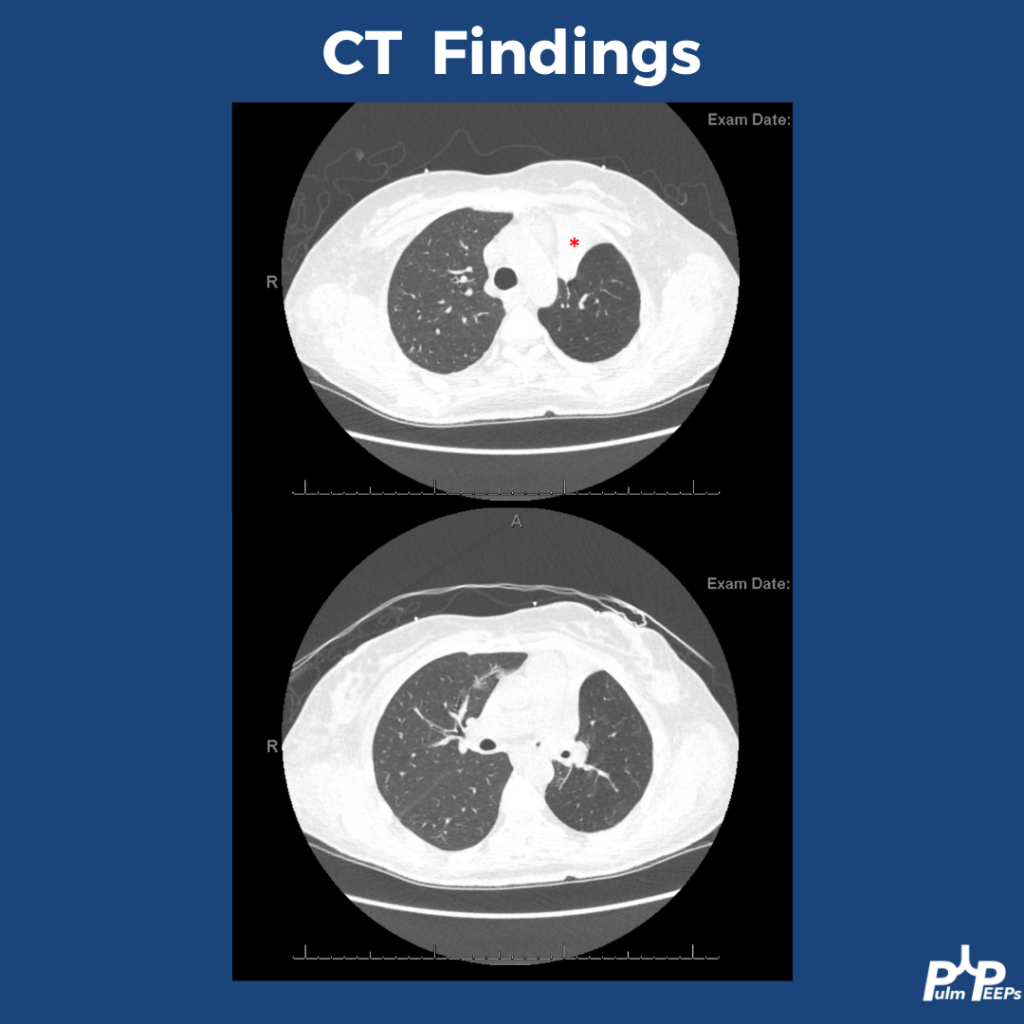
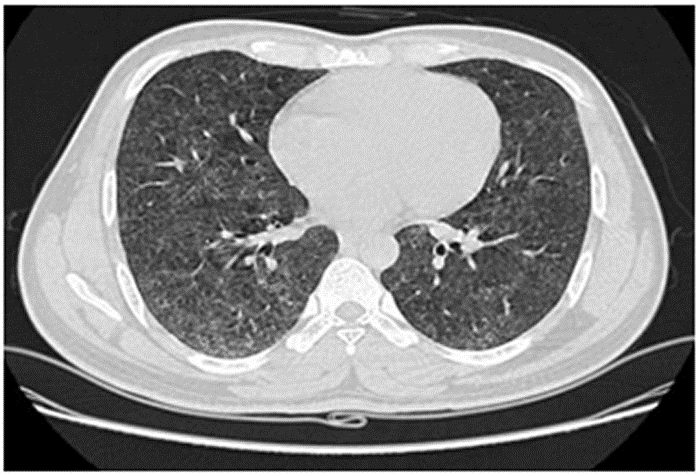
- Chest CT: Showed diffuse ground-glass opacities (GGOs) without fibrosis, consolidation, or lymphadenopathy.
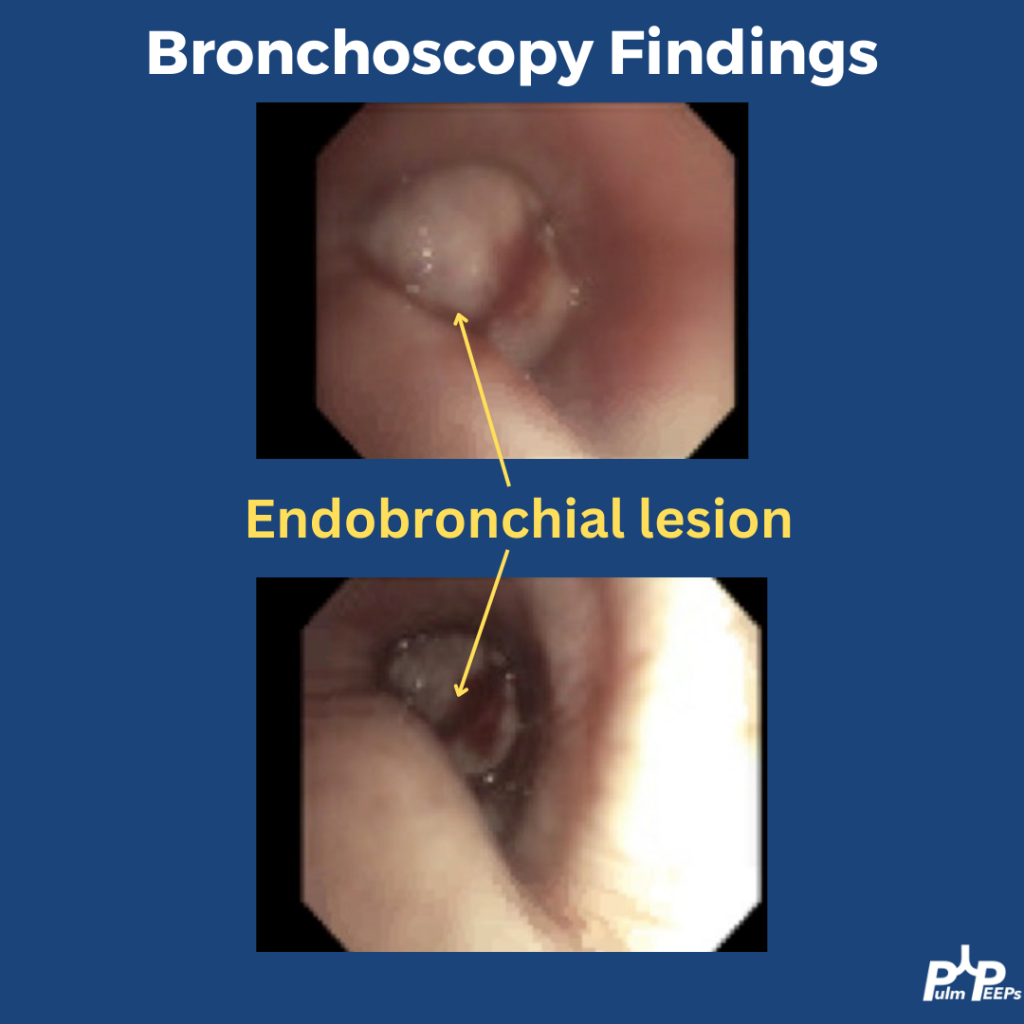
Imaging and Pathology

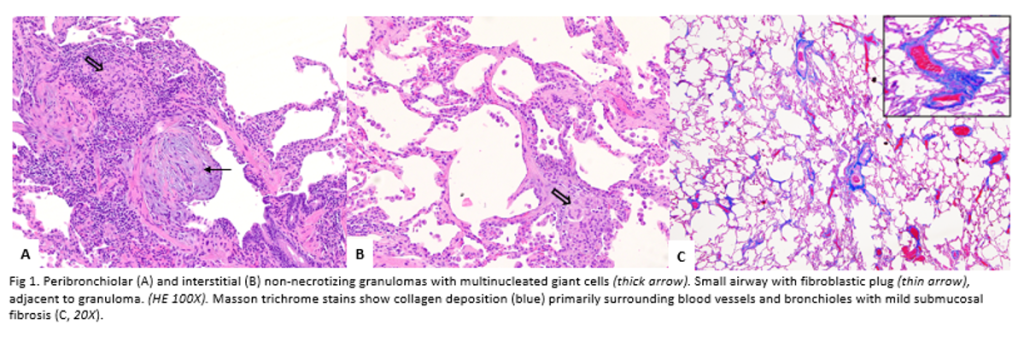
Pathology images a courtesy to Dr Isago Jerrett, pathology resident at RWJMS
Key Learning Points
Diagnostic Framework for Hypersensitivity Pneumonitis (HP)
- New classification: Based on fibrotic vs. non-fibrotic phenotype (not acute/chronic).
- CT features of HP:
- GGOs with lobular air trapping.
- “Three-density sign” (normal lung, low-density air-trapping, and ground-glass opacities).
- BAL: Typically shows lymphocytic predominance in chronic HP, neutrophilic in early stages.
- Serum IgG testing: Helps identify antigen exposure but doesn’t confirm disease alone.
- Lung biopsy (VATS): Revealed poorly formed granulomas and airway-centered inflammation—consistent with HP.
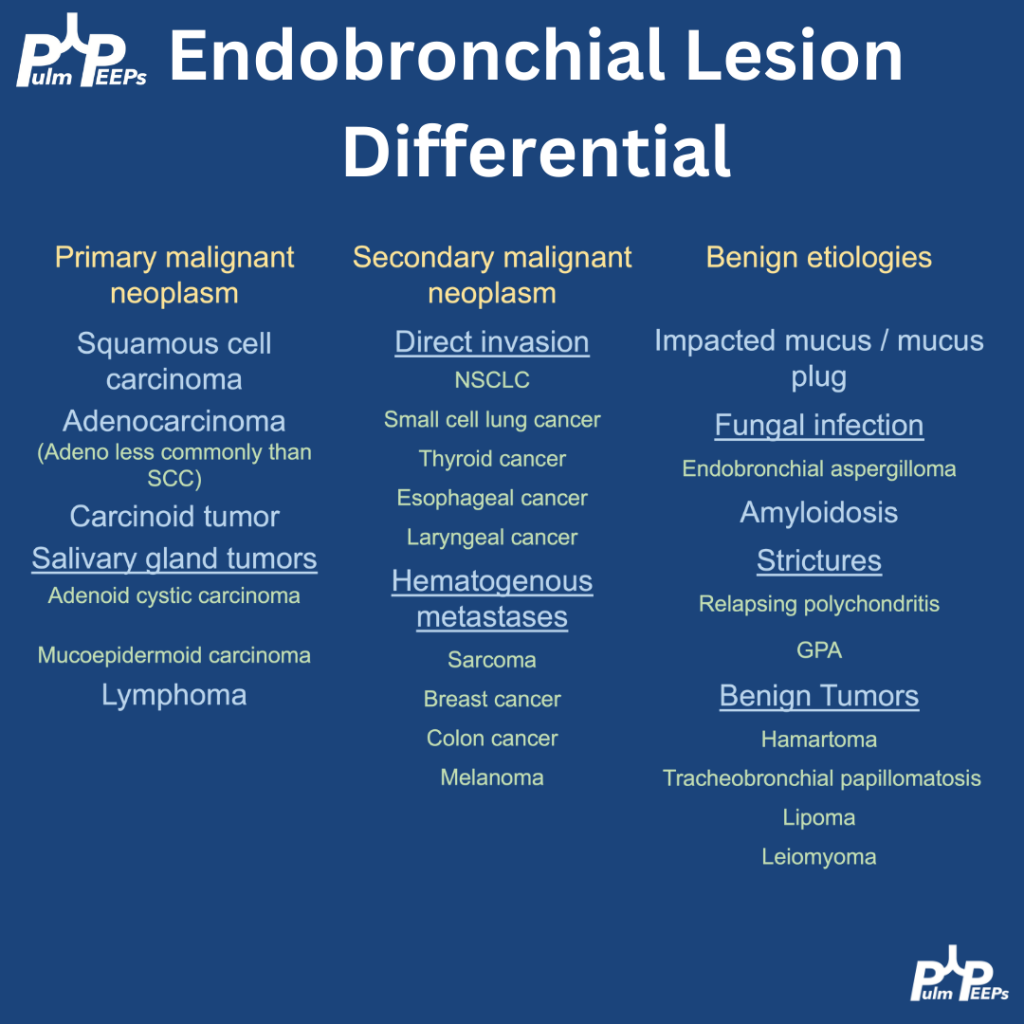
Differential Diagnosis of Granulomatous Disease
- Infectious: TB, fungal (must rule out with stains/cultures).
- Non-infectious: Sarcoidosis, HP, granulomatosis with polyangiitis.
- Key pathology clues for HP: Loosely formed granulomas, airway inflammation, giant cells.
Management and Outcome
- Primary treatment: Antigen avoidance (patient moved out of mold-exposed apartment).
- Adjunct therapy: Oral prednisone with a slow taper.
- Outcome: Symptomatic and radiographic improvement over six months.
Teaching Pearls
- Always take a detailed environmental and occupational exposure history.
- Hypoxemia with an elevated A–a gradient in a young adult should trigger concern for interstitial/parenchymal lung disease.
- CT and history are often enough to diagnose HP—biopsy is reserved for uncertain cases.
- Remember evolving terminology: think fibrotic vs. non-fibrotic HP, not acute/chronic.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More