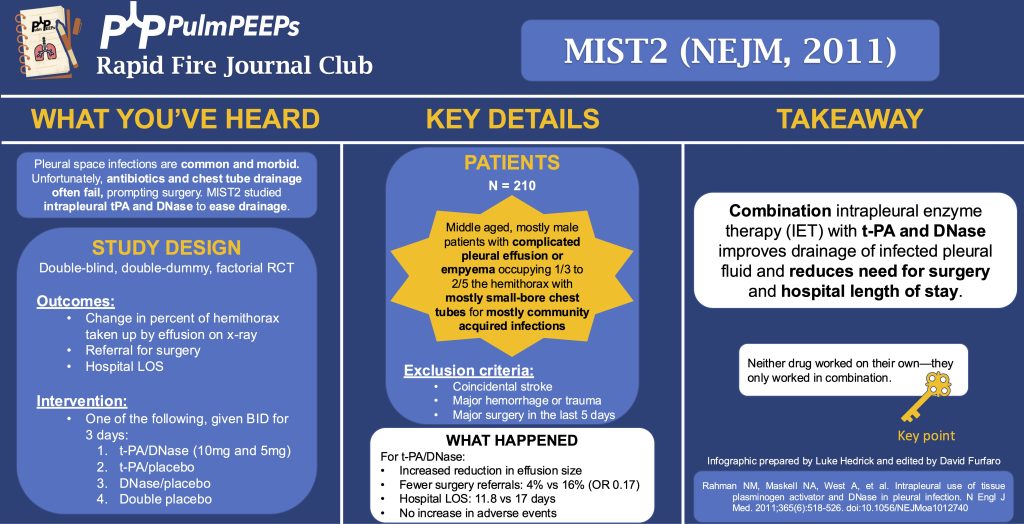
In this episode, we add another article to our Rapid Fire Journal Club. Luke Hedrick and Dave Furfaro discuss the MIST 2 trial published in NEJM in 2011 evaluating enzymatic therapy for complex parapneumonic effusions and empyemas.
Article and Reference
We are talking today about the MIST 2 trial evaluating the use of intrapleural tPa and DNase for intrapleural infections.
Key Learning Points
-
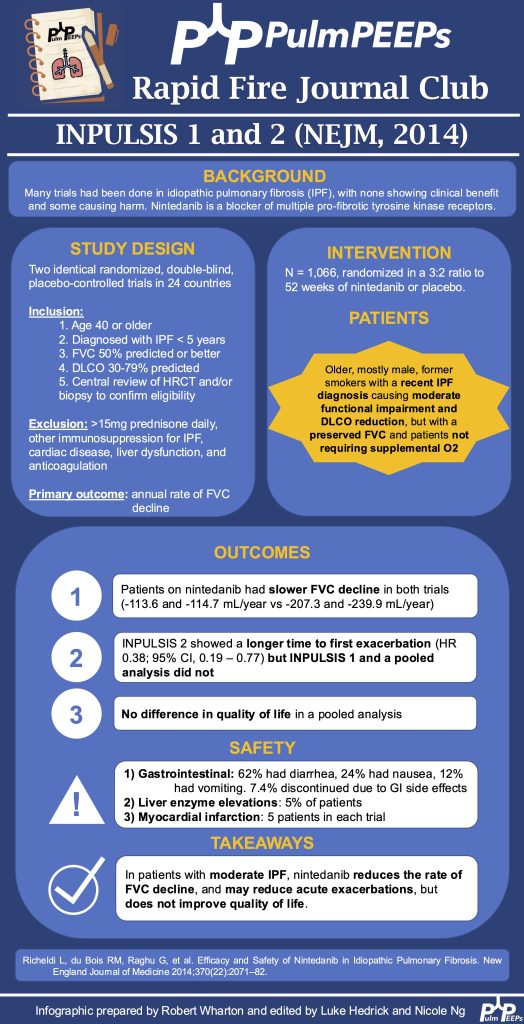
- Background:
- Infections in the pleural space are common and morbid, often requiring surgical intervention. Unfortunately, antibiotics and chest tube drainage often fail. The MIST1 trial (NEJM, 2005) of intrapleural streptokinase showed no benefit. MIST2 studied intrapleural tPA and DNase to ease drainage by breaking down septations and thinning pleural fluid.
- Study Design (design, primary outcome, participants, etc)
- Design:
- Double-blind, double-dummy, 2×2 factorial RCT at 11 UK hospitals from 12/2005 to 11/2008
- By double dummy, we mean that there was a sham placebo for each of the study drugs
- Double-blind, double-dummy, 2×2 factorial RCT at 11 UK hospitals from 12/2005 to 11/2008
- Primary Outcome
- Change in the percent of the hemithorax taken up by effusion on CXR at day 7 compared to day 1
- Key secondary outcomes:
- Referral for surgery
- Hospital LOS
- All cause 3 month and 12 month mortality
- AEs
- Participants
- Inclusion:
- Clinical evidence of infection (assessed by recruiting MD; EG, fever, CRP, WBC) and
- Pleural fluid with any of:
- Grossly purulent
- Positive pleural fluid culture or gram stain
- pH < 7.2
- Exclusion: aiming to exclude patients with increased bleeding risk or who can’t re-expand the lung after drainage
- Age < 18
- Previous intrapleural fibrinolytics, DNase, or both for empyema
- Allergy to tPA or DNase
- Coincidental stroke (hemorrhage risk)
- Major hemorrhage or trauma
- Major surgery in the last 5 days
- Previous pneumonectomy on the infected side
- Pregnancy, lactation
- Expected survival < 3 months from something other than what caused the pleural problem
- Summary: Middle-aged, mostly male patients with complicated pleural effusion or empyema occupying 1/3 to 2/5 hemithorax with mostly small-bore CDs for mostly community-acquired infections
- Inclusion:
- Design:
- Background:
Small-bore here meant < 15 Fr
- Intervention/Limitations
- N = 210 (193 analyzed) randomized approximately 1:1 to one of the following 4 arms:
- tPA/Dnase (10mg and 5mg)
- tPA and placebo
- DNase and placebo
- Double placebo
- N = 210 (193 analyzed) randomized approximately 1:1 to one of the following 4 arms:
-
-
- Medications were given BID for 3 days with clamping of the CD for 1 hour after each dose (to keep the drug in the pleural space)
-
- Outcomes/Safety
- Power: with N = 210 (actual analysis = 193), 80% power to detect 1 in 5 more patients with a 50% reduction in pleural opacity on CXR
- We’ll discuss the outcomes of tPA/DNase in combination because there was a highly significant interaction between the two (P = 0.002) for the primary outcome
- Efficacy:
-
-
- Primary (pleural effusion size reduction): -29.5% hemithorax vs baseline and -7.9% effusion size vs placebo (P = 0.005)
- Neither drug worked on their own
- Secondary:
- Referral for surgery: 4% vs 16% (OR 0.17, P = 0.03)
- Hospital LOS (excluding 391d outlier in placebo group): mean 11.8 vs 17 days (P = 0.006)
- Mortality: no difference
- Primary (pleural effusion size reduction): -29.5% hemithorax vs baseline and -7.9% effusion size vs placebo (P = 0.005)
-
-
- Safety:
-
-
- No difference in AE between groups
- 6 serious events across all groups, mostly related to bleeding (intra-pleural, GI, hemoptysis); other AE were made up of pain with drug administration, transient AMS, rash
-
- Takeaway
- Combination intrapleural enzyme therapy (IET) with tPA and DNase improves drainage of infected pleural fluid, and reduces need for surgery and hospital LOS
Infographic
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More