Hi everyone, we’re here with another Fellows’ Case Files. Today, we’re going virtually to Emory University School of Medicine. We’re joined by Associated Editor Luke Hedrick to dive into a critical care case. Listen in and let us know if you have any additional thoughts or questions!
Meet Our Guests
Luke Hedrick is a first-year pulmonary and critical care fellow at Emory University. He did his internal medicine residency at BIDMC in Boston. He is also one of our amazing Associate Editors here at Pulm PEEPs
Shirine Allam is an Associate Professor of Medicine at the Emory University School of Medicine where she is the Program Director of both the Pulmonary and Critical Care Medicine fellowship as well as the Critical Care Medicine fellowship. She completed her PCCM training at the Mayo Clinic in Rochester, followed by a Sleep Medicine fellowship at Stanford. She has received multiple teaching awards throughout her career
Case Presentation
A 32-year-old male is brought in by his coworkers unresponsive. He is a construction worker and was his usual self in the morning at the start of the day, but when they broke for lunch they noticed he was acting different—his arms were drooping, and while he initially was able to answer yes/no, he soon started babbling, then grunting, then vomited and became unresponsive. They laid him flat, threw cold water on him because it was 110 degrees and humid outside that day, and brought him to the ED.
When they arrive in the ED, he is unresponsive and warm to the touch. His vitals are notable for an oral temperature of 105, HR in the 160s, BP 76/34, a RR in the high 30s, and an SpO2 100% RA. His exam is relatively unremarkable other than for significant diaphoresis and both bowel and bladder incontinence.
Key Learning Points
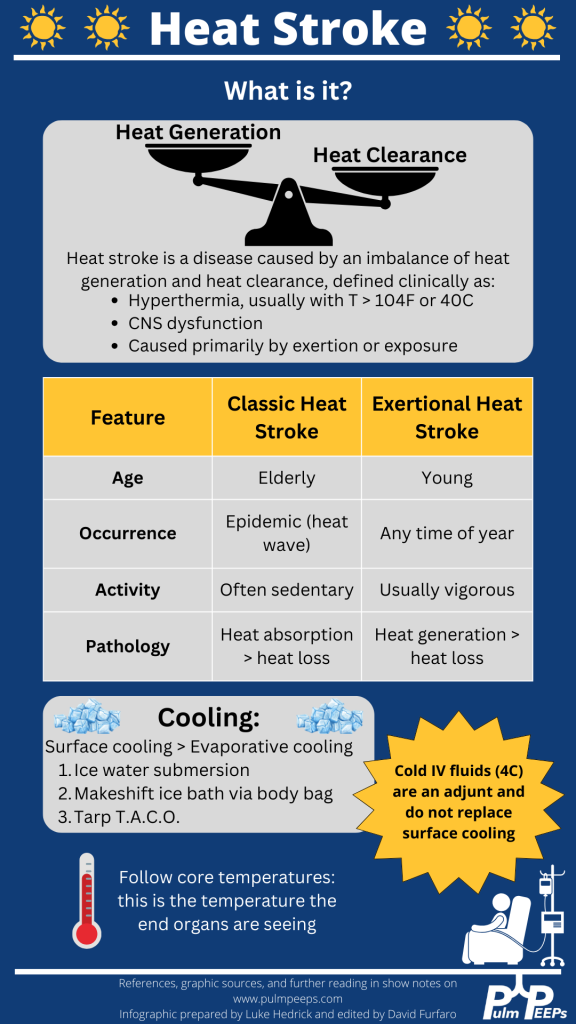
- Definition and recognition of heat stroke: Heat stroke is characterized by hyperthermia (>104°F or 40°C) accompanied by CNS dysfunction, primarily caused by exertion or exposure. Encephalitis without significant heat load does not constitute heat stroke.
- Management priorities: Rapid cooling is paramount to minimize long-term complications and organ failure. Cooling should be initiated as soon as possible, even before transportation to a hospital, particularly in cases of exertional heat stroke.
- Cooling methods: Surface cooling, such as immersion in ice water, is the most effective way to cool heat-stroke patients. Alternative methods include the TACO method and evaporative cooling, although they are less efficient. Refrigerated IV fluids can be used as an adjunct, but they do not replace the need for surface cooling.
- Monitoring and goals: Shivering during cooling should be monitored to prevent excessive heat generation. The goal is to reach a normal core body temperature (~38°C or 100.4°F). Traditional antipyretics like aspirin and acetaminophen should be avoided due to ineffectiveness and potential toxicity.
- Approach to endotracheal tube (ETT) exchange: ETT exchange requires preparation for potential complications. This includes ensuring the availability of airway equipment, sedation of the patient, and having additional personnel for assistance. Direct visualization using a video laryngoscope is recommended, along with measuring and marking the exchange catheter for proper insertion depth.
The following infographic can be downloaded from our website:
References and Further Reading
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More
