Today we’re kicking off another segment in our Guidelines Series, and doing a deep dive into the 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Over a series of episodes we’ll talk about the most recent updates to definitions around pulmonary hypertension, recognizing and diagnosing Group 1 – 5 pulmonary hypertension, risk stratification, and treatments. In this first episode, we will review the most recent definitions, including changes to the definitions that were new in 2022. We’ll then talk about recognizing and diagnosing pulmonary hypertension with tips and insights along the way.
Meet Our Co-Hosts
Rupali Sood grew up in Las Vegas, Nevada and made her way over to Baltimore for medical school at Johns Hopkins. She then completed her internal medicine residency training at Massachusetts General Hospital before returning back to Johns Hopkins, where she is currently a pulmonary and critical care medicine fellow alongside Tom. Rupali’s interests include interstitial lung disease, particularly as related to oncologic drugs. And she also loves bedside medical education.
Tom Di Vitantonio is originally from New Jersey and attended medical school at Rutgers, New Jersey Medical School in Newark. He then completed his internal medicine residency at Weill Cornell, where he also served as a chief resident. He currently is a pulmonary and critical care medicine fellow at Johns Hopkins, and he’s passionate about caring for critically ill patients, how we approach the management of pulmonary embolism, and also about medical education of trainees to help them be more confident and patient centered in the care they have going forward.
Infographic
Key Learning Points
- Why to have a high index of suspicion for pulmonary hypertension (PH)
- PH often presents subtly with slowly progressive dyspnea on exertion, fatigue, lightheadedness, exertional chest pain, or syncope.
- There’s often a delay of 1–2+ years from symptom onset to diagnosis, which is associated with worse mortality.
- Early recognition and treatment, especially for pulmonary arterial hypertension (PAH, WHO group 1), can significantly change outcomes.
- When to suspect PH
Think PH when:
- Dyspnea is out of proportion to:
- CT parenchymal findings (relatively normal lungs)
- Spirometry (normal FEV₁/FVC, volumes)
- There are subtle but progressive symptoms over months:
- Reduced exercise tolerance
- No obvious alternative explanation (e.g., no overt HF, CAD, big ILD, etc.)
- Physical exam may show (often late):
- Elevated JVP, V waves (TR)
- Peripheral edema, hepatomegaly, ascites
- Loud P2, RV heave
In the case: a woman with systemic sclerosis + slowly progressive exertional dyspnea + relatively normal CT parenchyma and spirometry → high suspicion.
- WHO classification: 5 PH groups (big picture + why it matters)
Used for pathophysiology, prognosis, and treatment choices:
- Group 1 – PAH
- Idiopathic, heritable (e.g., BMPR2), drug-induced (e.g., dasatinib)
- Connective tissue disease (esp. systemic sclerosis)
- Portal hypertension (portopulmonary HTN)
- HIV, HHT, congenital heart disease/shunts
- Rare: PVOD, PCH
- Group 2 – PH due to left heart disease
- HFrEF, HFpEF, valvular disease
- Most common cause worldwide.
- Group 3 – PH due to lung disease/hypoxia
- COPD, ILD, combined pulmonary fibrosis–emphysema
- OSA/obesity hypoventilation, chronic hypoxemia
- Group 4 – CTEPH
- Chronic thromboembolic pulmonary hypertension
- Group 5 – Multifactorial/unclear
- Sarcoidosis, myeloproliferative disorders, CKD, sickle cell, etc.
Patients can span multiple groups (e.g., systemic sclerosis: group 1 and/or group 3; sickle cell: many mechanisms).
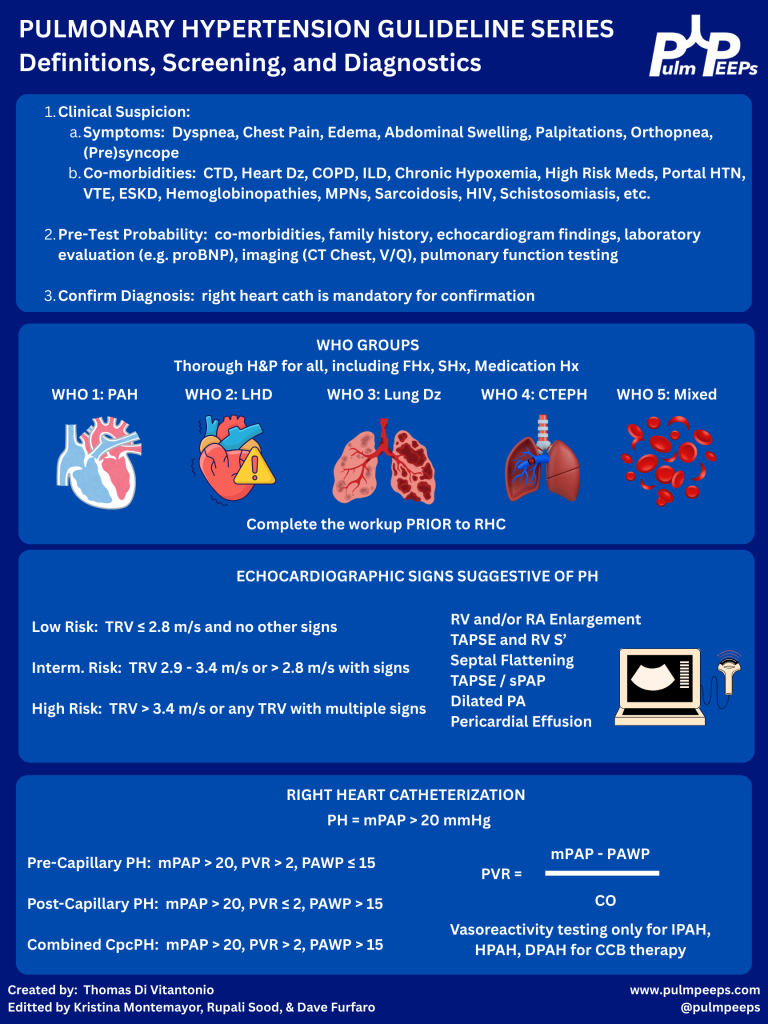
- Initial workup & refining pre-test probability
Once you suspect PH, you’re trying to answer:
- Does this patient likely have PH?
- If yes, what group(s) are most likely?
Core non-invasive tests:
- NT-proBNP (preferred over BNP)
- Surrogate of RV strain and prognosis.
- Normal value makes significant RV failure less likely.
- Oxygenation & exercise
- Resting SpO₂ plus ambulatory sats; consider 6-minute walk test.
- Exertional desaturation is common and clinically meaningful.
- CXR & ECG
- Low yield but may show RV enlargement, right axis deviation, etc.
- Pulmonary function tests
- Full set: spirometry, volumes, DLCO.
- Clue: isolated or disproportionately low DLCO with relatively preserved FVC suggests pulmonary vascular disease.
- Imaging
- High-res CT chest – parenchymal disease (ILD, emphysema).
- V/Q scan – best screening test for CTEPH; better than CT angiography for chronic disease.
- Sleep testing / overnight oximetry
- When OSA/nocturnal hypoxemia suspected.
- Echo: estimating PH probability (not diagnosis)
TTE is the key screening tool but does not diagnose PH.
Main elements:
- Peak tricuspid regurgitant (TR) velocity
- Used to estimate pulmonary artery systolic pressure (PASP).
- Categories:
- Low probability: TR velocity < 2.8 m/s, no other PH signs.
- Intermediate: 2.9–3.4 m/s ± other PH signs.
- High: > 3.4 m/s.
The presence and severity of TR ≠ TR velocity. You can have severe TR without PH.
- “Other signs” of PH/RV dysfunction on echo:
- RV enlargement or systolic dysfunction (qualitative, TAPSE < ~1.7 cm, S′ ↓)
- RA enlargement
- Septal flattening (D-shaped LV; systolic = pressure overload, diastolic + systolic = volume + pressure)
- Dilated PA
- Pericardial effusion
Interpretation pattern:
- Low pre-test probability + TR v < 2.8 + no other signs → PH unlikely.
- Intermediate TR v (2.9–3.4) + high pre-test probability and/or other PH signs → consider RHC.
- High TR v (>3.4) or clearly abnormal RV → strongly consider RHC if it would change management.
Also:
- Echo is great to follow RV size/function and PASP over time once PH is diagnosed and treated.
Case echo:
- TR velocity 3.1 m/s + mild RA enlargement + moderate RV enlargement + TAPSE 1.6 cm → intermediate probability, consistent with PH and RV involvement.
- Right heart cath (RHC): gold standard & updated definitions
You cannot definitively diagnose or classify PH without RHC.
Key directly measured values:
- RA, RV, PA pressures
- Pulmonary capillary wedge pressure (PCWP/PAWP) ≈ LVEDP
- Oxygen saturations in chambers/vessels
- Cardiac output (thermodilution)
Key derived values:
- Cardiac output (Fick)
- Pulmonary vascular resistance (PVR)
Updated hemodynamic definitions:
- Pulmonary hypertension (PH)
- mPAP ≥ 20 mm Hg (lowered from ≥ 25).
- Pre-capillary PH (think PAH, group 1; also groups 3, 4, some 5):
- mPAP ≥ 20
- PAWP ≤ 15
- PVR > 2 Wood units (new lower threshold)
- Isolated post-capillary PH (IpcPH) (group 2)
- mPAP ≥ 20
- PAWP > 15
- PVR ≤ 2
- Combined pre- and post-capillary PH (CpcPH)
- mPAP ≥ 20
- PAWP > 15
- PVR > 2
Rationale for the changes:
- Normal mPAP in healthy people is < ~19; 20 is about 2 SD above normal.
- Patients with mPAP 20–24 (esp. systemic sclerosis) already have worse outcomes than those < 20.
- Lowering PVR cutoff from 3 → 2 WU better aligns with these new thresholds and catches earlier precapillary disease.
Practical interpretation:
- You use mPAP + PAWP + PVR to:
- Confirm PH.
- Distinguish pre- vs post-capillary.
- Identify mixed disease.
- Echo tells you probability; RHC tells you what type and how severe.
- Vasoreactivity testing (acute vasodilator testing)
- Only indicated in:
- Idiopathic (IPAH)
- Heritable PAH
- Drug-induced PAH
→ Not routine for all PH patients.
- Performed in the cath lab with short-acting vasodilator (e.g., inhaled NO).
Positive test:
- ↓ mPAP ≥ 10 mm Hg
- To an absolute mPAP ≤ 40 mm Hg
- No fall in cardiac output
Why it matters:
- Identifies a small subset who can be treated with high-dose calcium channel blockers long-term and often have better prognosis.
- Does not predict response to other PAH therapies (ERA, PDE5i, prostacyclin, etc.).
- Screening high-risk populations
Some groups warrant systematic screening because of high PAH risk.
- a) Systemic sclerosis / systemic sclerosis spectrum
- Annual screening if:
- Disease duration ≥ 3 years
- FVC ≥ 40% predicted
- DLCO < 60% predicted
- DETECT algorithm (2-step):
- Step 1: uses labs and simple tests (FVC/DLCO ratio, NT-proBNP, autoantibodies, right axis deviation on ECG, telangiectasias).
- If positive → Step 2: adds echo (TR velocity, RA size).
- If high risk after Step 2 → RHC.
- Goal: catch early PAH before symptoms are severe.
- b) Other high-risk groups
Annual screening (usually with echo ± NT-proBNP, PFTs) for:
- Known heritable PAH mutations (e.g., BMPR2)
- Portal hypertension (esp. considering liver transplant or TIPS)
- HIV
Always layer this on top of clinical symptoms and progression.
- Big practical takeaways (what to apply on Monday)
- Don’t label “pulmonary hypertension” off CT or echo alone.
- Enlarged PA on CT or elevated PASP on echo ≠ diagnosis.
- RHC is required.
- Think PH early when:
- Dyspnea is out of proportion to imaging and spirometry.
- There is a relevant risk factor (systemic sclerosis, portal HTN, HIV, prior PE, congenital heart disease, etc.).
- Use the WHO groups to structure your differential and workup:
- Group 1 vs 2 vs 3 vs 4 vs 5 → drives what tests you order and what treatments you eventually consider.
- Echo = probability. RHC = truth.
- Echo gives you low / intermediate / high PH probability.
- RHC gives you pre- vs post-capillary, PVR, and hemodynamics needed for therapy.
- Know the new numbers:
- mPAP ≥ 20 = PH
- PAWP cutoff = 15
- PVR > 2 WU = precapillary component
- Don’t forget NT-proBNP, DLCO, V/Q scan, and high-risk screening (especially in systemic sclerosis and BMPR2 carriers).
References
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More
